|
|
|
Jarrod Shapiro, DPM
Practice Perfect Editor
Assistant Professor,
Dept. of Podiatric Medicine,
Surgery & Biomechanics
College of Podiatric Medicine
Western University of
Health Sciences,
St. Pomona, CA |
Normally as an editor of your Practice Perfect blog, I try to focus more on the "social" side of being a podiatrist. Occasionally, though, I have a clinical experience or topic that fires up my interest and forces me to write about it. Today's issue is one of those. It's not an especially complex one, but it has significant potential. Let's start our conversation with an abbreviated case study.
Case Presentation
This is the case of a 16 year-old Hispanic female who presented to my office about 2 years ago complaining of painful bilateral 1st metatatarsophalangeal joints and left arch pain. She was a long distance track runner who ran an average of 15-20 miles per week. Her pain was sharp in quality, located within the joint (rather than the medial eminence), 7/10, worse with walking and running, and better with rest. She also complained of focal left arch pain located at the navicular tuberosity. Her medical history was otherwise negative.
Figures 1 and 2 show her initial clinical and radiographic appearance. She had a fully flexible foot, including the first MTPJs. You'll notice the radiographs demonstrating the increased first intermetatarsal angle (15 degrees), mild hallux abductus interphalangeus deformity, and enlarged navicular tuberosity, with normal hindfoot architecture.
Figure 1
Preoperative appearance demonstrating
symptomatic left abducted hallux and bunion deformity. |
 |
Figure 2
Preoperative radiographs of the left foot. |
 |
For about 1 year, my treatment consisted of custom foot orthotics, shoegear changes, and the occasional NSAID. My patient did well for a short time, with complete resolution of her symptoms on the right side, but continued pain on the left. After discussion with the patient and her mother (she was now 17 years-old), we decided on surgical correction.
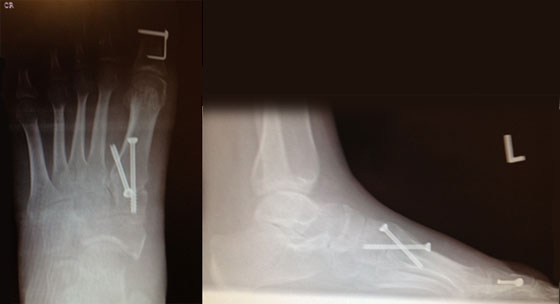
Here's where it starts to get interesting. You can tell from the postoperative radiographs that I performed a modified Lapidus bunionectomy, Akin osteotomy, and Kidner procedure. I also performed an endoscopic gastrocnemius recession for her gastrocnemius equinus.
Surgical Procedure Choice
I'll make a couple of comments regarding surgical procedure choice so we don't get too far off track. Her first IM angle wasn't huge but given her young age (propensity for more significant deforming forces), fused growth plate, increased first ray excursion, and elevatus on radiographs, I thought the Lapidus would be appropriate. I rarely perform Akins (I'm one of those that feels the Akin is a cheat when you fail to fully correct the IM angle), but this time, I decided to do it. I felt her equinus was significant enough to do a recession.
Here's the cool part. When I did her procedure, I completed the Lapidus and Akin without entering the 1st MTPJ at all. I didn't perform a capsulotomy; I didn't "rebalance" the joint in any way with capsulotendinous work of any sort. Essentially, I straightened the IM angle, plantarflexed the first ray a little, and corrected the bent hallux. You can see the results I obtained in figures 3 and 4. At over 1 year follow-up, the patient was completely pain free, continuing with her long distance running.
I'll focus your attention on the complete correction of her hallux valgus without entering the joint in any way (notice the hallux incision that ends distal to the 1st MTP joint, showing my lack of direct joint work). Additionally, the patient's range of motion immediately postoperatively and at every examination thereafter was better than her preoperative state. You all may be better surgeons than me, but the range of motion of the 1st MTPJ after head procedures in which joint work is done is always limited in dorsiflexion with a nonanatomical hard end range of motion. I've seen this not only in my own work but in the results of many other podiatric and orthopedic surgeons. I don't think it's just me.
Figure 3
Postoperative clinical appearance. |
 |
Figure 4
Postoperative radiographs. |
 |
You may argue that the Kidner and gastrocnemius recession may have had something to do with the results, and I won't argue that point. Additionally, this is a young patient with a highly flexible deformity. I'll agree with that too.
Here's what I think, though. In a flexible deformity without degenerative or significant adaptive joint changes, correcting the primary deformity (in this case the increased IM angle), deliberately staying away from the 1st MTP joint, will lead to better short and long term results. When we enter the 1st MTP joint with our dissection, the healing that occurs (irregular scarring unless continuous passive motion is instituted) causes significant joint limitation that is, in many (most?) cases permanent. By correcting the primary deformity without causing further damage, we successfully heal the patient rather than create new joint limitation.
Now, I don't think this is particularly amazing and unlikely to be original. However, after doing a Pubmed search, I was unable to find any study discussing this concept, what I'm calling the "extracapsular bunionectomy."
This makes me wonder about all those Austin bunionectomies so many of us do. Sure, it gets patients back to ambulation in regular shoes quicker. Certainly it's faster than other procedures. But is it better? Cases like this one bring up important questions that demand good research to answer. I'm hoping to start a prospective comparative study of the extracapsular bunionectomy to the Austin procedure in the near future. I'm told one of the fellowship programs will be presenting a poster along similar lines at the upcoming ACFAS conference, and if so, good on them! They'll deserve the credit for a potential paradigm shift in bunion surgery.
I urge you all to take an honest look at your surgical results and tell me that your Austin bunionectomies have full and complete unrestricted range of motion. I don't think you will be able to do that.
What do you think? Am I on to something important or is this all completely obvious and/or bogus? Do you disagree with my findings? Is it time for a paradigm shift in bunionectomies? Is it time for the extracapsular bunionectomy?
Best wishes.

Jarrod Shapiro, DPM
PRESENT Practice Perfect Editor
[email protected]
Get a steady stream of all the NEW PRESENT Podiatry
eLearning by becoming our Face book Fan.
Effective eL earning and a Colleague Network await you. |
 |
This ezine was made possible through the support of our sponsors: |
|