From last week's Part 1 of this case we received numerous excellent responses on the eTalk thread on this challenging patient. Below are listed several of your responses:
Bryan Markinson, DPM – I would consider these skin lesions that are nodules. I would seek initially to rule out a malignancy, and the bilateral nature leads me to put Kaposis Sarcoma at the top of the list. I would do a punch biopsy of each lesion, 3 mm. Pending the result, I would proceed to surgery after an oncology consult to make sure the problem was not already disseminated. Of course if it turns out not to be KS, the course of treatment would be tailored to the exact diagnosis. Both of these lesions are exophytic, therefore have little chance of reaching the bone, so MRI would be better for surgical planning, but ultrasound would be less expensive.
 Jeffery Kass, DPM – Prior to any surgical intervention I would order an MRI. One often can not tell how deep something travels or where it extends, I think it's important to have that knowledge to lessen any surprises. The MRI can tell you if there is bone involvement, if nerves or vessels are a component etc. Jeffery Kass, DPM – Prior to any surgical intervention I would order an MRI. One often can not tell how deep something travels or where it extends, I think it's important to have that knowledge to lessen any surprises. The MRI can tell you if there is bone involvement, if nerves or vessels are a component etc.
Carla Porter Pursnani, DPM – Does the patient have a history of HIV or is she of Mediterranean descent? Is there a history of a wound, a growth, history or family history of skin cancer?
From just the picture alone, the lesion on the right looks like it could be a wound with hypergranulation tissue due to lack of intervention, a granuloma, or nodular melanoma. The lesion on the left definitely looks cancerous, although I could put a neglected verruca on the differential list for completeness.
Speaking purely academically, ordering blood work, xrays and MRI along with biopsy are in order. Practically speaking, however, as a solo practitioner I would send her to a Moh's micrographic dermatopathologist, and assuming the biopsy comes out cancerous, an oncology consult based on the path report.
Alecia Williams, DPM – Looks like the beginnings of verrucous lymphedema or elephantiasis on the Left, tough to get rid of once those permanent lymphatic changes take place unless patient has major weight loss. Also have to exercise caution in doing any biopsy technique or excision as there is extensive skin tension and can cause a slow healing ulcer, more swelling to the area or another growth. Would use cryoablation to totally excise the one on the right and send to Path, again, would not subject patient to a preliminary incisional biopsy then excision because of the fragile skin.
Douglas Albreski, DPM – I’m hedging toward a benign condition. Eccrine poroma, usually solitary in nature, although I've seen multiple lesions. Literature relates to a condition when 15 or more are present. I will excise them and D and C the base times two with good results. Obviously send them to path, there is a known malignant variation of these lesions.
COURSE OF CARE
As many of you suggested, following the thorough clinical exam of this patient, there was a concern for malignancy, specifically of Kaposis Sarcoma (KS). The patient demonstrated no previous personal or family history of KS (or any other cancer). Lab work was obtained, including CBC, BMP, CRP, ANA, and all of these were essentially negative. An HIV test was performed and the patient was noted to be negative. Plain radiographs demonstrated no findings specific to the lesions. Due to the patient’s extreme claustrophobia, an MRI was not performed.
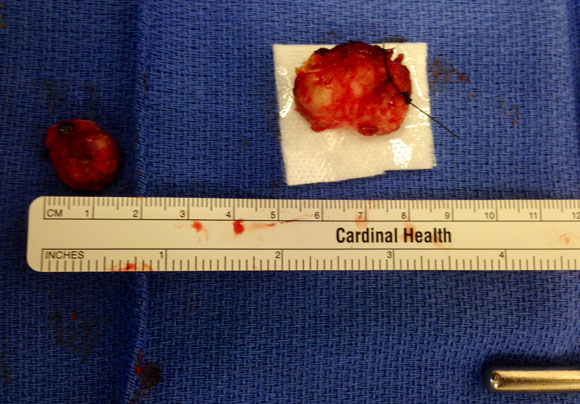
Despite the negative laboratory and imaging findings, the decision was made to perform excisional biopsy of both lesions and informed consent was obtained. These were performed in the operating room and each lesion was removed in total (Figure 1) and sent for fresh frozen section. The resultant pathology is shown below:
Figure 1
|
 |
|
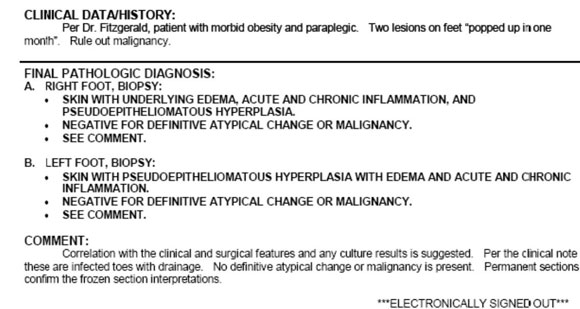
Pathology Report
|
 |
|
Upon confirmation of no malignancy, it was safe to proceed with wound closure in both biopsy locations. Considering the size of the lesions, the decision was made to perform local rotational flaps to provide soft tissue coverage over the resultant defects following biopsy. This decision was in deference to the tautness of the patients skin as a consequence of her lymphedema, and would thus allow for wound closure with relatively little tension by selective orientation of the flap geometry. On the right foot, the decision was made to perform a rhomboid-type closure – utilizing medial skin to close the defect (Figure 2a, b) – and on the left foot, a simple rectangular flap was performed (Figure 3).
Figure 2a, b
|

 |
|
Figure 3
|
 |
|
Upon completion of the procedure, compressive buttress dressings were applied bilaterally and continued supportive care for her paraplegia was initiated. The patient was connected with the lymphedema clinic and was set up with home lymphedema pumps for the ongoing management of this disease process. With regard to her feet, the patient demonstrated an uneventful postoperative course and her incisions healed without incident. To date she has had no further reoccurrence of either skin lesion.
DISCUSSION
There are many different elements of this case that we could discuss,. However perhaps the most germane (considering the overall negative malignancy) was the decision to perform excisional biopsy versus a less aggressive incisional biopsy or punch biopsy. For review, an incisional biopsy involves cutting into the lesion and removing a portion (but not all) of the lesion. If the lesion is found to be cancerous, further surgery may be needed to remove the whole abnormality. By contrast, in an excisional biopsy, the clinician generally removes the entire lesion. If the lesion of interest is large, an incisional biopsy may be performed to make sure the cosmetic outcome following the procedure is suitable. Alternatively, if the abnormality is small, an excisional biopsy may be performed. It is important to consider the anatomic location of the lesions as well as potential closure options prior to any intervention. In this case, I elected to perform excisional biopsy in both locations to remove the lesions in total. This was in consideration of their anatomic area, and due to my confidence that I would be able to obtain wound closure following complete excision with some element of a rotational flap or skin graft at each location to allow for primary closure.
While I am certain we could discuss the merits of one type of biopsy over another, it is perhaps most important to recognize the NEED to biopsy. I was told once during my residency training that I should “biopsy everything unless you know what it is for certain... and even then STILL biopsy, just to be sure.” There are many benign and malignant processes which manifest in the lower extremity, and it is important for clinicians involved in these patients to have a high index of suspicion and a low threshold for biopsy.
We love hearing from you. I would encourage you to share your insights, thoughts, and pearls on this case, and in general in eTalk section of PRESENT Podiatry.
All opinions expressed are my own and do not necessarily reflect those of my employer.

Get a steady stream of all the NEW PRESENT Podiatry
eLearning by becoming our Facebook Fan.
Effective eLearning and a Colleague Network await you. |
 |
This ezine was made possible through the support of our sponsors: |
|