|
|
|
|
Percutaneous Bunion Correction –
Are you kidding me? Not Anymore…
|
|
|
Reporting on clinical research done by
Guido LaPorta, DPM, MS
Chief, Foot and Ankle Surgery
Director, Podiatric Medical Education
Geisinger-Community Medical Center
Scranton, PA
Director, Podiatric Medical Education
Our Lady of Lourdes Memorial Hospital
Binghamton, NY
Director, Limb Salvage and Reconstructive Surgery Fellowship
Noman Siddiqui, DPM, MHA
Medical Director of the Center for Diabetic Limb Preservation
Division Chief of Podiatry
Rubin Institute for Advanced Orthopedics
Sinai Hospital, Baltimore, MD
Illustrations by
Joy Marlowe
Certified Medical Illustrator
LifeBridge Health, Rubin Institute for Advanced Orthopedics
|
|
|
|
|
In this remarkable and ground breaking lecture, Drs Guido LaPorta and Noman Siddiqui present their review of 135 of their cases of a minimally invasive bunion procedure employing modifications of existing technique that they have found to be most successful. During this 30 minute lecture, Dr LaPorta demonstrates the technique using clear illustrations, followed by intraoperative photographs and video of the procedure being done, providing excellent teaching for all who care to consider adopting the procedure.
Dr LaPorta begins by reviewing the regional variations on bunion procedures currently being done in America. He considers the goals of bunion surgery, of reducing the IM angle, reducing elevatus of the hallux, reducing frontal plane rotation, reducing hypermobility/instability, preserving range of motion and providing some form of internal fixation in such a way that you can mobilize the joint post-op as soon as possible. Their hypothesis is presented that they can best meet these goals via a percutaneous, minimally invasive distal osteotomy procedure that would provide equivalent results to the more traditional open procedures being done today, ie, Lapidus, Austin, Mitchel, SCARF, and that by doing the procedure with minimal dissection, the procedures would result in less loss of ROM and a patients would be able to return to shoes quicker.
Dr LaPorta is one of those unique individuals, those great scientists, who has an open mind that will not be closed. He never stops observing, even after conclusions are drawn. He was a keen observer of the minimal incision surgery (MIS) movement during the 80s and did see a few results using these techniques which met the goals listed above and were in fact, he felt, excellent. Of course, we also know there were many less than optimal results. But it was these good results that compelled him to continue to explore how these techniques could be performed to yield consistently excellent outcomes.
Dr LaPorta was influenced largely by work done by Weinberger et al in 1991, and Giannini in Bologna Italy in 2003, both of which reported high patient satisfaction and better results with less surgery associated morbidity than the open procedures commonly being done in much larger numbers. Giannini has reported on a total of over 1000 procedures1.
Dr LaPorta adopted Radwan and Mansours 2013 procedure2, and completed a series of 135 cases that he reports on in this lecture. He postulates that due to the lack of soft tissue dissection, you get “quick and complete formation of periosteal proliferation, healing the osteotomy”. He has shown a series of remarkable results.
The only fixation that he uses is a Steinman pin retrograded into the 1st metatarsal shaft for four weeks, which serves to maintain the lateral translation of the metatarsal head capital fragment and stretch the soft tissue to adapt to its new more rectus position. Dr LaPorta explains that this fixation is more than adequate because you haven't destabilized the 1st MPJ by detaching all the soft tissue, periosteum and ligaments, as is commonly done in open HAV procedures. The procedure now takes him seven minutes to perform.
|
|
|
|
|
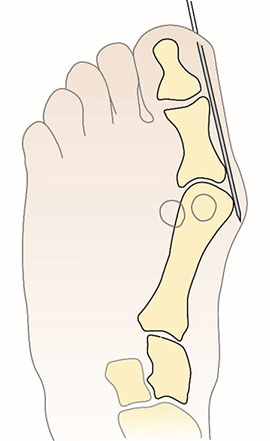
Figure 1. A and B, Insert pin from distal tip of great toe subperiosteally to metatarsal head. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
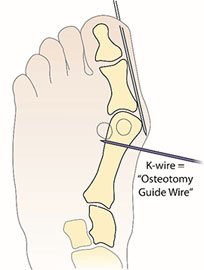
Figure 2. A and B, Place 1.8-mm axis guide wire at metatarsal neck. C, Use additional wires to create multiple drill holes. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
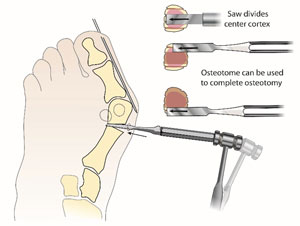
Figure 3. Use osteotome (A and B) or mini micro sagittal blade (C) to complete osteotomy. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
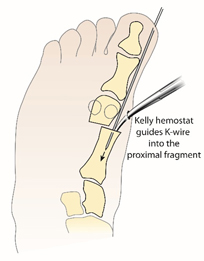
Figure 4. A and B, Kelly hemostat guides K-wire into the proximal fragment. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
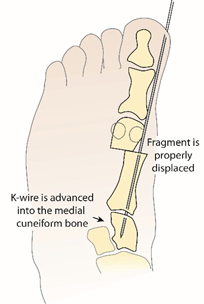
Figure 5. A, K-wire advanced into the medial cuneiform bone. B and C, Wire placement and reduction are confirmed on AP (B) and lateral (C) view fluoroscopic images. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
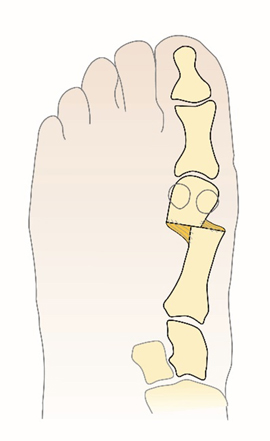
Figure 6. Illustration (A) and radiograph (B) show bone after consolidation is achieved. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
Figure 7. A, Preoperative radiograph shows mild hallux valgus. B, Postoperative radiograph obtained at 2.5-year follow-up. Reduction has been maintained. Note the remodeling of the medial shelf. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
|
|
Figure 8. A, Photograph obtained before treatment shows hallux valgus deformity. This is the same patient that is shown in Figures 1 through 6. B and C, Photographs obtained 6 months after surgery. The hyper-pigmented skin on the lateral view photograph denotes the site of the incision. D, Excellent range of motion was maintained at the first metatarsophalangeal joint. Copyright 2015, Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore.
|
|
|
|
|
###
- A minimally invasive technique for surgical treatment of hallux valgus: simple, effective, rapid, inexpensive (SERI). Int Orthop. Giannini S1, Faldini C, Nanni M, Di Martino A, Luciani D, Vannini F. 2013 Sep;37(9):1805-13. doi: 10.1007/s00264-013-1980-8. Epub 2013 Jul 3
- Percutaneous distal metatarsal osteotomy versus distal chevron osteotomy for correction of mild-to-moderate hallux valgus deformity. Arch Orthop Trauma Surg. Radwan YA1, Mansour AM., 2012 Nov;132(11):1539-46. doi: 10.1007/s00402-012-1585-5. Epub 2012 Jul 22.
- Siddiqui N, LaPorta G. Emerging Insights On Minimally Invasive Hallux Valgus Correction. Podiatry Today.2014;27(9).
- Hallux Valgus Correction: An Alternative Approach, Abstract Poster, ACFAS 2015 Annual Conference.
|
|
Get a steady stream of all the NEW PRESENT Podiatry eLearning by
becoming our Facebook Fan.
Effective eLearning and a Colleague Network await you.
|
|
This ezine was made possible through the support of our sponsors:
Grand Sponsor
Major Sponsor
|
|
†Approved for 19 CME/CECH Credit Hours
 This activity has been planned and implemented in accordance with the standards and requirements for approval of providers of continuing education in podiatric medicine through a joint provider agreement between the Kent State University College of Podiatric Medicine and PRESENT e-Learning Systems. This activity has been planned and implemented in accordance with the standards and requirements for approval of providers of continuing education in podiatric medicine through a joint provider agreement between the Kent State University College of Podiatric Medicine and PRESENT e-Learning Systems.
PODIATRISTS: The Kent State University College of Podiatric Medicine is approved by the Council on Podiatric Medical Education as a provider of continuing education in podiatric medicine.The Kent State University College of Podiatric Medicine has approved this activity for a maximum of 19 continuing education contact hours.
 MDs/DOs: Professional Education Services Group (PESG) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. MDs/DOs: Professional Education Services Group (PESG) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Professional Education Services Group (PESG) designates this live educational activity for AMA PRA Category 1 CreditsTM. Physicians should only claim credit commensurate with the extent of their participation in the activity. A maximum of 19 AMA PRA Category 1 CreditsTM will be awarded.
NURSES: Professional Education Services Group (PESG) is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation. PESG is awarding a maximum of 19 contact hours for this activity.
|
|
|