|
|
|
|
Radiowave Surgery for Matrixectomy
|
|
|
|
|
|
|
A great percentage of patients that present to a podiatrist with a foot problem have an ingrown toenail. Risk factors predisposing to development of ingrown toenails include anatomic and behavioral mechanisms. Some experts suggest that wider nail folds and thinner, flatter nails increase the risk of ingrown toenails, but this remains unproven. A case-control study with 46 patients found no difference in the anatomic shape of toenails in patients with and without ingrown toenails1. Repetitive trauma (eg, running, kicking) or inadvertent trauma (eg, stubbing the toe) may also be inciting factors.
|
|
|
Surgical procedures are well documented in the literature beginning in 1869, as described by Wood in Lancet. Podiatric physicians have an excellent reputation among the medical community for correcting nail deformities. Surgical removal of the nail fold and matrix with a scalpel and sutures, CO2 laser matrixectomies, phenol matrixectomies, etc, have all been used in the podiatry office with varying levels of success. Surgical matrixectomy often creates long disability, prolonged healing and difficulty wearing shoes. Chemical matrixectomy with phenol also has long term healing with weeks of drainage and pain. In addition, phenol (carbolic acid, hydroxybenzene, monohydroxybenzene, benezoil) is a highly caustic chemical and is also known to be a VOC (Volatile Organic Compound). Phenol vapor is known to be harmful to the eyes, skin, respiratory system, digestive system, heart, kidney, liver, and lung. Phenol is readily absorbed through the skin and with inhalation. In the United Kingdom, phenol is listed as a hazardous chemical and classified as a human carcinogen, requiring significant controls for use, storage, and disposal. Using a CO2 laser has a significant learning curve and many times, due to the vaporization of tissue, also has a lengthy healing time.
|
|
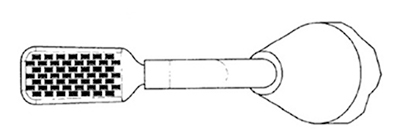
In my practice, radiowave surgery (BNA ISURG ) has replaced all of the above methods. Some of the advantages include minimal bandaging, low reoccurrence rate (2%), quick return to normal shoes, and significantly less drainage and/or pain. In addition, the cost of the radiowave device and electrodes is low. In 1978, Maness, et al2 found that 3.8 MHz was the optimum power for cutting soft tissue. The high frequency device quickly gained acceptance in dentistry and thereafter podiatry. Then in 1985, a novel electrode was developed by Dr Jon Garito (Figure 1) which was partly bare and partly insulated to selectively direct the electrosurgical current to the appropriate tissue (eg matrix).
 Figure 1: Early Electrodes
Figure 1: Early Electrodes
|
|
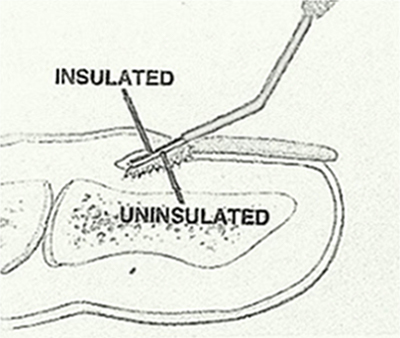
On these early electrodes, the bare metal exposed side was smooth brass. The problem with this smooth metal design is that the radiowave energy flows to edges of the metal and does not flow to the middle. So the doctor needs to continually turn the matrix electrode for the edges to fully ablate the cells. In the design of the advanced matrix electrode, the metal (Figure 2) is now roughened with micro points instead of being smooth. This roughened surface provides an even distribution of radiowave energy over the surface of the metal spade electrode, thus ablating the matrix cells in a more efficient and consistent manner. The reason the radiowave energy is more efficient and consistent is due to the "edge effect” in physics. The radiowave current flows to the edges or the points now created on the metal surface.
|
|
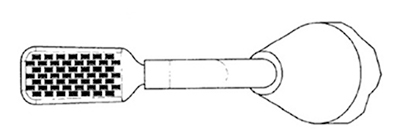 Figure 2: New BNA Electrode
Figure 2: New BNA Electrode
|
|
|
The procedure is basically the same as with all podiatric matrixectomies. Using a digital block with plain lidocaine and a digital tourniquet, the offending nail margin is removed with nail cutting forceps. Using the BNA electrode with the projections surface facing the matrix, the unit is turned on in the cut mode for two seconds. This is repeated one time. The area may be lightly phenolized, although I have found this unnecessary. A topic antibiotic and small sterile bandage is applied. The patient is instructed to remove the bandage before the next shower and cover with a clean one. The patient may return to normal shoes and normal activity.
|
|
|
|
|
The radiowave technique has been successfully used in podiatric, dermatology, and family practice medicine for many years. The new BNA Advanced Matrix electrodes seem to improve and simplify the matrixectomy procedure in the treatment of ingrown toenails. Radiowave matrixectomy also provides the patient with a rather easy surgical procedure to recover from.
|
|
|
###
-
Pearson HJ, Bury RN, Wapples J, Watkin DF. Ingrowing toenails: is there a nail abnormality? A prospective study. J Bone Joint Surg Br. 1987;69(5):840-842.
-
Maness WL, Roeber FW, Clark RE, et al. Histologic evaluation of electrosurgery with varying frequency and wave form. Journal of Prosthetic Dentistry. 1978;40(3):304-308.
-
Kendall MW. Podiatry Management. May, 2008.
-
Antrum RM. Radical Excision of the Nail Fold for Ingrowing Toenail. The General Infirmary, Leeds LS1 3EX, England. January, 1984.
-
Hettinger DF, Valinsky MS, Nuccio G, Lim R. Nail matrixectomies using radiowave technique. JAMPA 1991;81(6):317-321.
-
U.S. Patent 4,517,975.
- Brown JS. Radiosurgery. In: Minor Surgery a Text and Atlas. 4th ed. London, England: Arnold; 2000.
-
Pollock SV. Electrosurgery of the skin. New York: Churchill Livingstone; 1991.
|
|
This ezine was supported by an educational Grant from:
|
|
|

 Figure 1: Early Electrodes
Figure 1: Early Electrodes