
Residency Insight
Oral Antibiotics for Osteomyelitis – Is it Time?
Oral Antibiotics for Osteomyelitis – Is it Time?

Medical care provided by physicians is critical to therapeutic success against osteomyelitis. The Oral Versus IV Antibiotics (OVIVA) clinical trials studied whether oral antibiotics would be as effective as IV antibiotic therapy in cases of complex orthopedic infection, including osteomyelitis. Adult patients were recruited from multiple centers throughout the UK where they received their care for a bone or joint infection. The NIH funded this study.
It has been a longstanding view ever since the 1970s when Waldvogel’s classic article mentioned “… osteomyelitis is rarely controlled without the combination of careful, complete surgical debridement and prolonged (four to six weeks) parenteral antibiotic therapy…”1 that adults with bone and joint infections “need” prolonged IV therapy for optimal treatment. But this is inconvenient, expensive, and may not make sense, since many antibiotics are well absorbed orally. After many have testified against this theory, and others attempted studies to disprove it, the OVIVA group set out to challenge the assumption that intravenous antibiotics are necessary. A meta-analysis by Conterno et al involving 180 patients with chronic osteomyelitis showed no advantage of intravenous over oral therapy.2 However, there was insufficient evidence to draw conclusions about potential clinical utility due to the high risk of bias for these trials given various deficiencies in trial design and conduct. The OVIVA study, therefore, set out to conduct a non-inferiority trial to evaluate outcomes at 1 year after oral vs intravenous therapy during the initial 6 weeks of treatment for orthopedic infections.
The OVIVA Study Concluded that after Surgical Intervention, Oral Antibiotics are Non-Inferior to IV Antibiotics for the Treatment of Osteomyelitis
The primary composite end point, definite treatment failure within 1 year, was defined as the presence of at least one clinical, microbiologic, or histologic criterion of failure. Of the 1054 total patients enrolled from 26 UK centers, the most common organism was Staphylococcus aureus and the second most common was coagulase-negative staphylococci, followed by streptococci, pseudomonas, other gram-negative rods, and culture-negative infections involving the lower extremities. The method of choosing the specific antibiotic was made by the infectious diseases experts who devised and tailored the therapy for each patient; adjunctive rifampin and follow-on oral therapy were allowed.
The duration of therapy was a median of 78 days in the intravenous group and 71 days in the oral group, as the researchers allowed continued antibiotic therapy past 6 weeks. Seventy-six percent of participants continued their antibiotic therapy past 6 weeks. A sensitivity analysis was performed according to surgical procedure. Although the numbers were small and the results not significant, better outcomes were associated with oral therapy than with intravenous therapy among participants who did not undergo debridement, and better outcomes were associated with intravenous therapy than with oral therapy among patients who underwent debridement with implant retention or single-stage revisions. Patients who were treated with intravenous therapy had a median length of hospital stay that was 3 days longer and more often discontinued therapy because of intravenous catheter complications than did patients who received oral therapy. There were no significant between-group differences in the incidence of Clostridium difficile infection (1.7% in the intravenous group and 1.0% in the oral group) or serious adverse events.
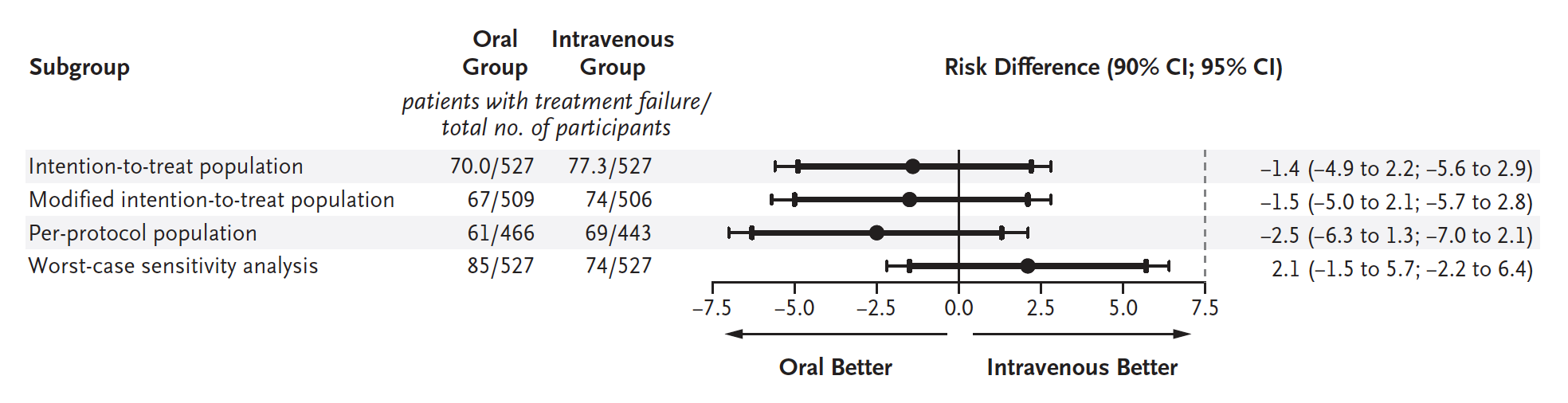
The primary analysis included 506 participants who were randomized to intravenous antibiotics and 509 who received oral antibiotic treatment, all within 6 weeks of developing the infection. At 1-year follow-up, the rate of failed treatment was 14.6% in the IV group and 13.2% in the oral group. The difference in the risk of definitive treatment failure was -1.4 percentage points, which satisfied the non-inferiority margin of 7.5 percentage points. While catheter complications occurred more frequently with the IV patients, the rate of serious adverse events otherwise was not significantly different between the two groups.
Now here is what this all means: Oral therapy was clearly non-inferior to IV. These results held up in several sensitivity analyses, including something we called a “worst case” outcome. Take a look at this chart from the article to sum up some of their findings.
This is great news, right? The oral approach to treating osteomyelitis will be safer, just as effective, and save healthcare dollars. That sounds wonderful. However, this study is not as much of a knock-out as it may seem.
Keep in mind, this study does not isolate specific antibiotics, nor is this study advocating oral antibiotics for osteomyelitis without surgical intervention. For a study to make claims of a cure for osteomyelitis, there would need to be bone biopsies confirming the presence and absence of infected bone before and after antibiotic treatment. Rather, this study simply claims that after surgical intervention, oral antibiotics are non-inferior to IV antibiotics.
For those desiring guidance for specific antimicrobial regiments for specific organisms, this study won’t do that. However, my recommendation is that you continue to use the antibiotic of your choice: the one you know will cover the identified microbes. Consider using a highly bioavailable oral antibiotic for the treatment of the bone and joint infection at hand. To answer the original question – “is it time for oral antibiotics for the treatment of Osteomyelitis?” - it is premature to recommend a widespread switch to oral therapy for osteomyelitis. However, we are definitely moving a step in that direction. With more trials to come, it may make what currently seems like a leap of faith into a clear and sound evidence-based decision.
-
Waldvogel FA, Medoff G, Swartz MN. Osteomyelitis: a review of clinical features, therapeutic considerations and unusual aspects. N Engl J Med. 1970 Jan 22;282(4):198-206.
Follow this link -
Conterno LO, Turchi MD. Antibiotics for treating chronic osteomyelitis in adults. Cochrane Database Syst Rev. 2013 Sep 6;(9):CD004439.
Follow this link -
Li HK, Rombach I, Zambellas R, et al. Oral versus Intravenous Antibiotics for Bone and Joint Infection. N Engl J Med. 2019 Jan 31;380(5):425-436
Follow this link



Comments
There are 1 comments for this article
The experimental Chaskin procedure that I invented was used to treat a patient with gangrenous, osteomyelitis digits using dermoscopy during surgery with powdered antibiotics. IV antibiotics was not that helpful without podiatric surgery using polarized light. Angular dependency with such polarized light is helpful during the healing process. Not only was a transmetatarsal amputation avoided as well as a leg amputation, the toes healed and began growing back longer. If anyone wants info regarding the experimental Chaskin procedure. 718 417 4895 Lastly we all should be grateful to present podiatry for helping all of us during this covid 19 virus tragedy.