Residency Insight
A Surgeon’s Thoughts When Prescribing Opioids
A Surgeon’s Thoughts When Prescribing Opioids

There have been some growing pains recently regarding the opioid abuse epidemic. We as surgeons have a difficult decision that we have to make with every procedure no matter how invasive: How do we address this patient’s pain and how much is too much or too little? Let’s face it, there is a clear challenge to determine what is the responsible number of opioids to prescribe, check and update the Controlled Substance Utilization Review and Evaluation System (CURES), and give an appropriate amount to actually provide pain relief to patients.
Max Out Your Regional Block
A Level I prospective, randomized comparison study done by Schipper et al out of Foot & Ankle International in 2017 took a look and compared an intraoperative ankle block versus a single-shot popliteal fossa block as primary anesthesia for forefoot operative procedures. In their study, they looked at a total of 167 patients with 88 patients receiving an ankle block (AB) and 79 patients receiving a single-shot popliteal fossa block (PFB). The ankle blocks were performed by injecting a total of 50 mL of 0.25% bupivacaine in equal amounts (10 mL) around the five major ankle nerves that supply innervation to the entire foot. They discuss use of an ultrasound only to identify the posterior branch of the tibial nerve because of its variable course and relation to the artery. They also performed a single-shot PFB the same way for all patients using ultrasound guidance. A separate injection of the saphenous nerve was administered when indicated by the operative approach. The analgesic effect of the PFB lasted significantly longer (20.9 hours) when compared to the ankle block (14.5 hours). They concluded that patients who received a PFB had significantly better pain management and decreased opioid requirements in the immediate peri-operative period than patients who received an ankle block. This study helps us to see that with appropriate and accurate regional anesthesia we can effectively reduce the requirement for oral pain medications.1
The use of appropriate and accurate regional anesthesia can effectively reduce the requirement for oral pain medications
Acetaminophen as Effective as Tramadol
Helmerhorst et al performed a non-inferiority randomized controlled trial out of the Netherlands, published in JBJS in 2017 to determine whether prescription of acetaminophen is non-inferior to acetaminophen and tramadol after operative treatment of an extremity fracture. Fifty-two patients were randomized and assigned by computer random number generation into two groups with the two different post-operative oral pain regimens. Blocking was used to balance the magnitude of the surgical procedure: relatively small (hand, wrist, foot, or clavicle) and relatively large (shoulder, elbow, knee, ankle, or hip). Patients with multi-trauma, pelvic fractures, pathologic fractures, stress fractures, pregnant, or breast-feeding were excluded from the study. At discharge post-operatively, patients were prescribed their perspective medications to be taken as needed for two weeks. At inclusion, patients were asked to rate the pain intensity using an 11-point ordinal scale. Two weeks post-operatively, all patients completed a questionnaire that included a rating of their overall satisfaction with pain relief.
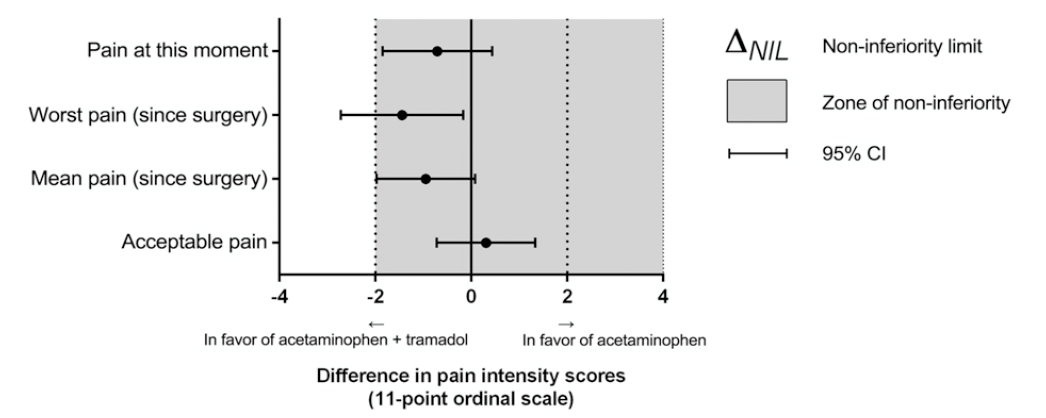
The conclusion of this study is that prescription of acetaminophen is not inferior compared with acetaminophen and tramadol in patients who underwent operative treatment for an extremity fracture. Some limitations of this study in regards to those that are foot and ankle surgeons exclusively, is that the fractures, although limited to the extremities, does not exclude non-foot and ankle fractures. Since tramadol is potentially habit-forming and has more side effects, the use of just acetaminophen is worth the consideration for the sole oral pain medication for the post-operative treatment of extremity fractures.2
Acetaminophen is not inferior compared with acetaminophen and tramadol in patients who underwent operative treatment for an extremity fracture
How Much is Too Much?
Often times the question comes up of how much pain medication should be prescribed. I have seen practitioners say “give them three weeks of narcotics, I don’t want to have to hear the patient complain” and I have also heard, “I don’t want to give this patient any narcotics, this procedure shouldn’t hurt them too much”. There are two studies regarding the opioid utilization in orthopedic patients. The first one is a level II prospective study by Saini et al, and interestingly, of 988 patients following an outpatient foot and ankle surgical procedure, narcotics were overprescribed by nearly twice the amount that were actually consumed. They looked at risk factors that lead to increased opioid consumption and surprisingly, those risk factors included: regional block anesthesia, younger age (<60 years), preoperative pain, and continuous infusion catheter. They also noted that there was a large residual standard error, which they attributed to an unexplained variance of opioid consumption that they observed in their particular patient population. The standard error is a statistical term which essentially measures the accuracy with which a sample represents a population.3
The other study published in JBJS in 2018 was a Level IV prospective evaluation looking at the opioid consumption in 1,513 patients following non-operative treatment of fractures with or without dislocation, of the entire body. Physicians were asked to continue their normal prescribing patterns during the study period. Most of the prescribing doctors opted for non-steroidal anti-inflammatory drugs (NSAIDs) as their first choice, and opioids were reserved for those patients with moderate or severe pain. The opioids prescribed in the study included Percocet(r), codeine with ibuprofen, or 100-mg sustained-release tramadol. They found a significant difference between the high and very high daily alcohol consumption groups in terms of patient-reported opioid consumption. This study reveals a direct correlation between opioid use and daily alcohol consumption.
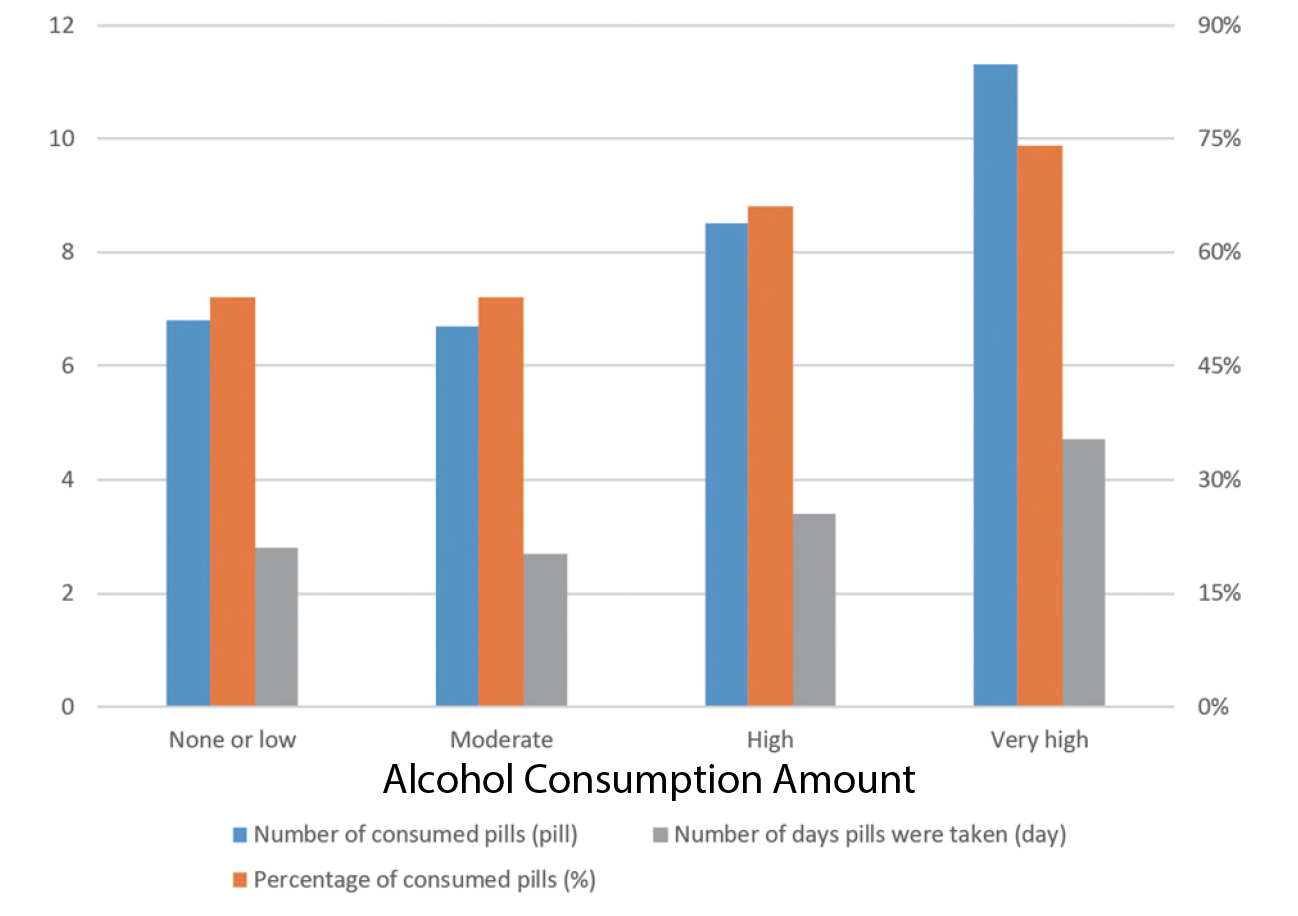
The study showed higher opioid consumption and for more days in patients with fractures with or without dislocations of the wrists or ankles compared to any other part of the body. Compared to the 50% consumption of opioids in the study by Saini, this study found that over 70% of patients were prescribed more opioids than actually used. Of all of the locations of the injury studied, interestingly the ankle had one of the highest number of pills consumed while the foot had the least amount of pills consumed. Lastly, one of the major limitations of this study was that it was performed at one hospital in China. These results should be carefully applied to other sociocultural regions of the world.4
This study reveals a direct correlation between opioid use and daily alcohol consumption
As surgeons we face a challenging task of balancing pain relief with generalizable pain management guidelines. With these studies, we can see that there is a lot that may be attributed to the epidemic, without any solid concrete answers available. After considering the type and location of injury, surgeons should consider prescribing the smallest dose for the shortest time and not use a shotgun approach for all fractures. Each patient is unique with different co-morbidities, alcohol history, and the type and location of fractures, which all may impact the effects of oral pain medications.
In conclusion:
- Regional blocks aid in decreasing the consumption of opioids post-operatively. Popliteal fossa blocks are more effective than ankle blocks.
- Acetaminophen alone is not inferior to acetaminophen with tramadol in treating pain after surgical fixation of extremity fractures.
- Over 50-70% of prescription opioids for orthopedic injuries are going unconsumed.
- Alcohol may decrease the sensitivity of patients to oral opioids for relieving pain, possibly explaining why Zhu et all found there was increased use of opioids in those patients that have increased daily alcohol consumption.
-
Schipper ON, Hunt KJ, Anderson RB, Davis WH, Cohen BE. Ankle block vs single-shot popliteal fossa block as primary anesthesia for forefoot operative procedures: prospective, randomized comparison. Foot Ankle Int. 2017 Nov;38(11):1188-1191.
Follow this link -
Helmerhorst GT, Zwiers R, Ring D, Kloen, P. Pain relief after operative treatment of an extremity fracture: a noninferiority randomized controlled trial. J Bone Joint Surg Am. 2017 Nov 15;99(22):1908-1915.
Follow this link -
Saini S, McDonald EL, Shakked R, Nicholson K, Rogero R, et al. Prospective evaluation of utilization patterns and prescribing guidelines of opioid consumption following orthopedic foot and ankle surgery. Foot Ankle Int. 2018 Nov; 39(11):1257-1265.
Follow this link -
4. Zhu H, Gao Y, Zhang C, Zheng X. A prospective evaluation of patient-reported opioid utilization after nonoperative treatment of fractures and dislocations. J Bone Joint Surg Am. 2018 Jul 18;100(14):1177-1183.
Follow this link



Comments
There are 0 comments for this article