
Paths to Practice Perfection
Innovations to Address Challenges in Closure of Foot and Ankle Chronic Wounds
Innovations to Address Challenges in Closure of Foot and Ankle Chronic Wounds
Surgeons and wound care specialists are constantly looking for the quickest method to close hard to heal chronic wounds. This has resulted in the trial and error of a variety of different methods and products based on clinical experience to close these challenging chronic wounds. Clinical experience dictates, not every closure method is appropriate. We recently started utilizing the ZipLine Medical product in these difficult to close chronic wounds as it is simple and adaptable for most patients with these challenging chronic wounds.
The foot and ankle present unique challenges to chronic wound closure. These include:
- Poor vascularization and perfusion
- Limited subcutaneous fat and thin skin
- Multiple articulating joints and high wound edge tension
- In the diabetic patient, associated vascular insufficiency and neuropathy
- Diabetic foot ulcers are traditionally difficult to close, with a high incidence of reoccurrence and dehiscence
The most common methods of acute incision closure are sutures or staples. However, these introduce several challenges:
- Percutaneous insult in already compromised tissue.
- High focal force along the suture thread or staple wire, resulting in strangulation of sensitive tissue, ischemia and necrosis. Staples may trigger nickel allergies.
- Lack of wound protection from tension and distraction forces.
- Scar quality and application speed of sutures are highly variable and skill dependent.
- Removal of both require a provider visit and can be uncomfortable for the patient.
The ideal wound closure might indeed be non-invasive, easy to use, cost-effective, fast, reliable, repeatable, and provide relief from wound edge tension, insult and strangulation. The Zip Surgical Skin Closure device from ZipLine Medical (Campbell, CA) has effectively addressed this for surgical procedures and is being used increasingly for foot and ankle surgical incision closure. It has been clinically proven to reduce closure time, produce better outcomes and reduce wound-related complications. But what is really exciting for the chronic wound care physician is a new product called PreLoc from ZipLine that is based on the successful Zip device but addresses the unique needs of the chronic wound. It leverages the non-invasive nature, ease of use and adjustable closure features of the Zip, but in a format that is optimized to effectively offload tension and incrementally close a wide variety of chronic wounds.
As with staples and sutures for acute wound closure, traditional methods for chronic wound closure have been less than ideal. In the past we have used DermaClose tissue expansion devices or retention sutures for approximating wound edges. However, these can either cause new wounds to form in the delicate peri-wound tissue and can often be less reliable. We began to use the PreLoc device from ZipLine about a year ago and our results have been outstanding. Before we present a case study demonstrating our results, let's discuss the benefits of this device. Simply put, the PreLoc Wound Closure addresses the needs of an ideal wound closure device.
These are:
- Non-invasive: no percutaneous insult to peri-wound tissue. PreLoc uses a large hybrid hydrocolloid and acrylic skin adhesive patch to attach to the skin and spread the tension forces.
- Uniform closure force and protection from distraction: the PreLoc structure acts as a cage or scaffold, protecting wound edges from tension and acute distraction forces.
- Versatile, adjustable, compatible with standard wound care: PreLoc's closure mechanism consists of infinitely adjustable and reversible zip-tie straps which may be temporarily removed for incision or wound debridement or application of biologics or dressings. It can be used in conjunction with total contact casts as well.
- Based on proven technology and clinical evidence: PreLoc is based largely on the Zip Surgical Skin Closure device, which has over 16 clinical studies demonstrating both clinical and economic benefits. The Zip has seen rapid adoption for acute closure of all types of surgical wounds and lacerations.
- Sized for the task: PreLoc is available in both 2cm and 5cm formats; the versatile design allows application on high contour foot and ankle wounds, and the new application method greatly enhances the ease of use for the busy wound care physician.
- Tenacious: The hydrocolloid and acrylic base adhesive combination enables wear time of one to three weeks, depending on the wound and patient. We have used the adhesive without needing Mastisol or compound tincture of benzoin for most non-plantar surfaces, and on plantar surfaces or areas where the device may see additional wear and tear, we've typically applied these agents for good measure, and it's worked well.
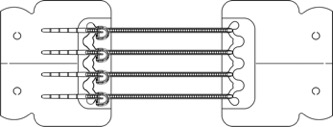
Here is what the device looks like out of the sterile package. The straps are spaced 1cm apart, and the gap between the two adhesive bases is approximately 5cm. Each adhesive base can be applied separately, which gives us the flexibility to treat the wound and plan where the second side will be placed. It can also be cut into two smaller devices to facilitate application in complex contours, although we have not had the need to use this feature. The straps can be tightened, loosened, and completely removed from the wound bed for periodic treatment and application of biologics or dressing materials.
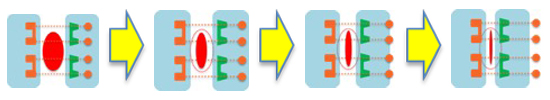
The mechanism of action is similar to traditional external tissue expansion devices, and it promotes the "linearization" of the wound, which has been shown to facilitate effective closure.

Case Study
The Charcot Foot diabetic ulcer is one of the most difficult and challenging type of ulcer to heal. The following patient case review is becoming an increasingly common patient we see in our clinics. With the use of the innovative Zipline Medical product we were able to meet many of these wound closure challenges and heal this chronic ulcer in four weeks.
58-year-old Male with Past Medical History (PMH)
of Type 2 Diabetes
- History of right Charcot Arthropathy
- Full thickness plantar ulceration present for over 1 year
- s/p Plantar Exostectomy preformed 10 months earlier
- s/p right Gastroc Recession performed 2 months ago
- s/p Left Partial 4th and 5th Ray resections 2 years ago
- ESRD on dialysis
- Off loaded via Air Cast, non-tolerable to TCC
Initial presentation - 3.0 x 1.3 x 0.4cm
Amniotic product applied and Preloc
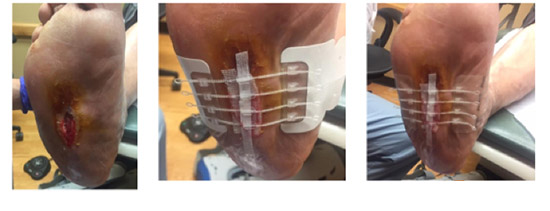
2 weeks later - 1.3 x 0.6 x 0.3 85% closure

3 weeks post - 1.4 x 0.5 x 0.1 96% closed from original and 70% closed in the past week
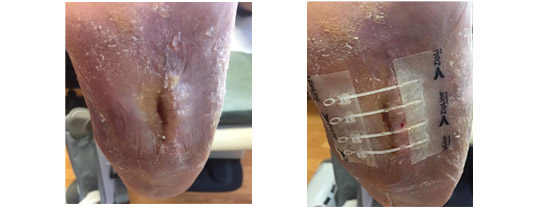
4 weeks from Initial presentation - Closed

Although our use of this product is relatively new, we have effectively been able to close wounds in weeks, where traditional methods of treatment and closure would have taken months (if at all), so we are very excited to continue to use this product.
Regards,
Matthew Garoufalis, DPM, CWS
Professional Foot Care Specialists
5241 S. Cicero Ave.
Chicago, IL 60632



Comments
There are 1 comments for this article
This does seem like a useful alternative to ex-fix for those chronic Charcot wounds. I would worry about some of my patients walking on this. Can it be placed under a TCC?