Residency Insight
Is Surgery Necessary for Unstable Ankle Fractures in Diabetic Patients? - A Review
Is Surgery Necessary for Unstable Ankle Fractures in Diabetic Patients? - A Review
Reference
Lovy AJ, Dowdell J, Keswani A, Koehler S, Kim J, Weinfeld S, Joseph D. Nonoperative versus operative treatment of displaced ankle fractures in diabetics. Foot Ankle Int. 2017 Mar;38(3):255-60.
Link to Original Article
https://www.ncbi.nlm.nih.gov/pubmed/27923219
Design/Level
Level 3 Retrospective Comparative Series
Intro
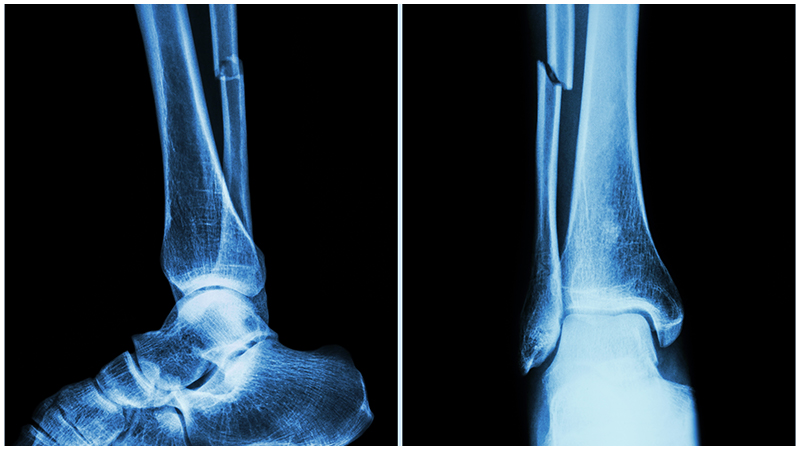
Patients with diabetes are at a high risk of complications with foot and ankle injuries given their potential vascular compromise, neuropathy, and high sugar levels. There is limited literature on complication rates of diabetic patients with foot and ankle trauma. This begs the question if ankle fractures should in fact be repaired surgically for patients with diabetes. This study aims to describe: 1) outcomes and complications of non-operatively treated displaced ankle fractures in diabetics and 2) compare non-operative and operative treatment for displaced ankle fractures in diabetics.
Patients/Methods
- Retrospective medical record review from September 2011 through December 2014 for all ED ankle fracture consults
- Inclusion criteria: >18 years old, a displaced ankle fracture defined as widened mortise on injury film with intact soft tissues and a physician-documented diagnosis of diabetes mellitus or a diagnosis was made according to the American Diabetes Association criteria, patients initially evaluated by Ortho staff at their hospital with min 3 visits within 3 months
- Exclusion criteria: open fractures, polytrauma, nonambulatory status, and prior ipsilateral lower extremity
- 28 patients with displaced diabetic ankle fractures, 20 treated non-operatively, 8 treated operatively
- 7 months (3-18 months) follow up
- Non-operative follow up of min 3 weeks or operatively ORIF within 21 days
- No patients had preoperative diabetic ulcers present
Results/Discussion
This study found a complication rate of 75% in non-operative group v. 12.5% in operative group. Complications of non-operative treatment were loss of reduction/malunion, new onset Charcot, cast ulcer, unplanned surgery (unintended ORIF), deep infection. This demonstrated that there is a 21x increased chance of complication in non-operative treatment compared to operative treatment (P = .004). The most common complication found was loss of reduction/malunion. Further analysis of patients showed that there is significantly higher complication rate among dialysis-dependent patients (14-fold increased odds of complications compared with operative treatment (P = .027))
Conclusion
The authors conclude that there is an unacceptably high complication rate with non-operative treatment of displaced diabetic ankle fractures compared to operative treatment. Given this, open reduction internal fixation should be performed to afford better functional outcomes for these patients
Relevance
Ankle fractures in diabetic patients remain challenging due to their high complication rates with or without surgical intervention. Previous literature has shown that patients who underwent nonoperative treatment did well after ankle fractures. Other studies show the high risk of complications, including infection, malunion, and Charcot. This is the largest case series of this kind to bring to light nonoperative v. operative treatment of ankle fractures in the diabetic population. They followed the patients for 7 months, which may be a limitation to see arthritic changes in the population. However, this follow up time helps us determine nonunion and delayed union, which was one of their primary outcomes. Although this study is relatively small, they had appropriate power analysis, revealing 92.6% power to detect a significant difference with our study size. This study showed an unacceptably high complication rate with non-operative treatment of displaced diabetic ankle fractures compared to operative treatment. This brings to light the importance of treating ankle fractures in diabetic patients surgically.
Link to Original Article
https://www.ncbi.nlm.nih.gov/pubmed/27923219



Comments
There are 0 comments for this article