
Practice Perfect 713
Can We Compress the Legs of Patients with CHF?
Can We Compress the Legs of Patients with CHF?
Treating venous leg ulcers and edema is a very common situation for many lower extremity specialists. These disorders are complex because they involve a number of comorbidities, including congestive heart failure (CHF). One of the issues I have witnessed over the years involves the concern that applying significant compression to the legs of patients with either chronic or acute CHF exacerbations will lead to a worsening of the disorder. The thought process, here, is that the limbs are acting as a third space, holding extra fluid that the heart is unable to circulate, and pushing that fluid back upward will tip a patient into worsening heart failure.
This idea is a little simplistic because it doesn’t take into account other potential causes of limb edema such as chronic renal disease and hypoalbuminemia (both of which may be comorbid with CHF). Since gradient compression is the mainstay for venous leg ulcers and most causes of lower extremity edema, it is important for us to know if it is safe to apply compression to the limbs in these patients.
And that is the question for today’s Practice Perfect: In patients with congestive heart failure, is compression of the lower extremities a safe practice?
Before we examine the research, take a quick look at the graphic below for a very basic refresher on cardiac output. For our purposes, we’ll focus more on the stroke volume side of the equation, specifically venous return and, to a lesser extent, systemic vascular resistance, since compression may theoretically increase the vessel resistance in the legs. Patients with chronic heart failure have decreased cardiac output (for reasons we will not discuss here) and end up with decreased “output” (less blood pumped from the heart) and decreased “input” (less blood able to enter the heart with subsequent congestion in the lungs, liver, and extremities).
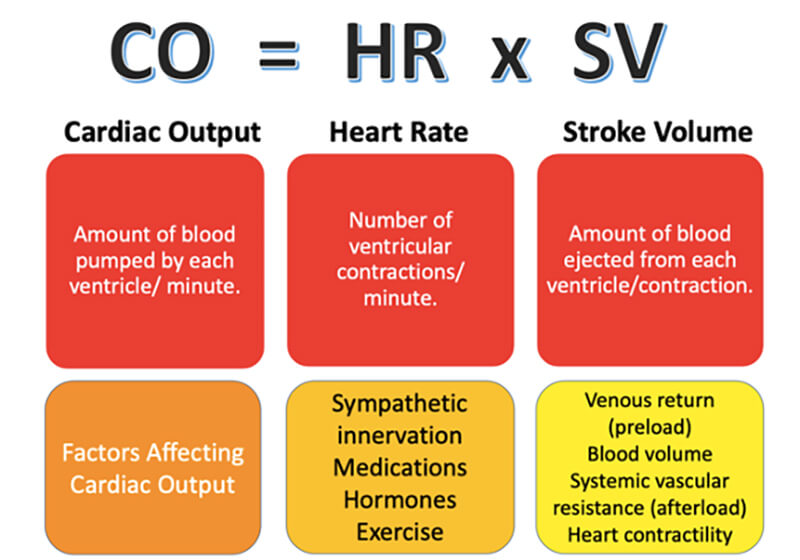
Now, if our lower extremity compression therapy (be it by pneumatic pumps or dressings) made heart failure worse, we should expect to see a decrease in cardiac output. In 2014, Bickel and colleagues1 looked at 19 patients with heart failure from systolic dysfunction. They applied intermittent sequential pneumatic compression sleeves to these patients (maximum pressure 50mmHg at a rate of 2 cycles/second) and tracked various cardiac parameters before, during, and after compression. At the start of the study, the baseline mean left ventricular ejection fraction was 32% (< 40% is abnormal) and mean cardiac output was measured as 4.26 L/minute.
These researchers found that during compression therapy, cardiac output increased from 4.26 to 4.83 L/min, a statistically significant finding. They also found stroke volume increased from 56.1 to 63.5 mL without an increase in heart rate. This stroke volume increase occurred as a result of decreased vascular resistance. Ejection fraction increased by 3%, which was not statistically significant. None of the patients experienced symptoms either during or after the treatment.
There are a couple of things we should consider with this study. First, the pneumatic compression system provided a pressure of 50mmHg, greater than that applied by an Unna boot (30mmHg2), multilayer compression system (40mmHg at the ankle and 17mmHg at the knee2), or compression stockings (15- 40 mmHg depending on the prescription). It is fair, then, to extrapolate the results of this study to our venous disease patients undergoing compression therapy for leg ulcers. If a pneumatic pump doesn’t cause decompensated heart failure, then a compression garment won’t. Additionally, patients in the Bickel study underwent bilateral compression, with a beneficial effect. Unilateral compression – commonly used when a unilateral leg ulcer is present – will have even less of an effect on the heart.
In February 2020 Attaran, et al also examined this issue with a retrospective cohort study of 95 patients with heart failure who underwent compression therapy for venous disease.3 They tracked various outcomes including mortality, weight gain, admissions for CHF decompensation, and the use of diuretics. In all of these endpoints, they found them to be no different between the compression therapy patients and heart failure patients in general.
Finally, in March of 2020 comes a consensus statement from 15 international experts about the use of compression therapy.4 Among the 21 recommendations was one about use of compression in heart failure patients. They recommend against using compression in New York Heart Association class IV heart failure (severe disease in which the patient is unable to carry on activity without discomfort with heart failure symptoms at rest) and recommended against use in NYHA class III (limitation of activity with comfort at rest) but they didn’t provide a rationale for this recommendation. They recommended cautious use in these patients in specific situations and with clinical monitoring.
I find it a little difficult to agree with these recommendations because much of the research they cite to justify these recommendations saw little to no worsening of outcomes with the use of multilayer compression therapy. These studies did not see a worsening of cardiac insufficiency, pulmonary edema, or indices of left heart function.
Given that the physiology of using compression therapy (improved cardiac output) supports its use, and the majority of outcomes studies show no adverse effects, it seems the evidence is on the side of safely using common leg compression methods. However, given the lack of highly powered studies and the consensus statement’s somewhat conservative cautions about using compression in severe heart failure patients, it seems appropriate to at least take a team-based approach to those patients with the most severe heart failure and start a discussion with their cardiologist and other medical doctors before proceeding. It’s most likely safe, but careful monitoring and understanding our patient’s comorbidities will always be beneficial.

-
Bickel A, Shturman A, Sergeiev M, Ivry S, Eitan A, et al. Hemodynamic effect and safety of intermittent sequential pneumatic compression leg sleeves in patients with congestive heart failure. J Card Fail. 2014 Oct;20(10):739-746.
Follow this link -
Blair, SD, Wright, DD, Backhouse CM, Riddle E, McCollum CN. Sustained compression and healing of chronic venous ulcers. BMJ. 1988 Nov 5:297:1159-1161.
Follow this link -
Attaran RR, Cavanaugh A, Tsai C, Ahmad T, O’Chaar C, et al. Safety of compression therapy for venous ulcer disease in the setting of congestive heart failure. Phlebology. 2020 Feb 6;268355520905178.
Follow this link -
Rabe E, Partsch H, Morrison N, Meissner MH, Mosti G, et al. Risks and contraindications of medical compression treatment–A critical reappraisal. An international consensus statement. Phlebology. 2020 Mar 2;268355520909066.
Follow this link






























Comments
There are 1 comments for this article
I had two heart attacks in 2012. About three years ago I learnt about HERBAL HEALTHPOINT and their successful herbal protocol for Coronary Artery Disease and Heart Failure, the herbal protocol is a miracle. Go to their web page w w w. herbalhealthpoint. c om. Its been years since this herbal treatment, my artery is clear and no sign of a heart attack. I do lots of walking and lost some weight too