
Practice Perfect 750
Let’s Talk TMA - The Hopeful Amputation - Part 1
Let’s Talk TMA - The Hopeful Amputation - Part 1

At first blush you might think an editorial about the transmetatarsal amputation is a bit dark. However, I’d like to suggest that this is not the case. In fact, when it comes to diabetic foot infections, gangrene, and the horrible family of maladies affecting the foot this is, perhaps, my favorite procedure. Before judging me too harshly, I’ll explain.
We never want to amputate any part of the foot, much less the entire distal forefoot. Undergoing procedures involving loss can be psychologically difficult for patients. Patients are most often in a hospital with an acute complication when this procedure is performed, and they may have entered the hospital with what originally appeared to be, to them, a more or less normal foot and then left the hospital having lost a significant part of their body. This is true and difficult.
But when you examine diabetic foot complications with a little more nuance, you’ll see that “keeping the toes” may not be as good for patients as it may seem. First, we have to remember that any patient with a diabetic foot ulcer, much less infection, gangrene, or Charcot have what is rightly called malignant diabetes. Their disease has progressed to a point where it is worse than some cancers with a high likelihood of ending their lives prematurely.1,2 Second, recall that it takes both neuropathy and deformity to create an ulcer,3,4 almost universally the sentinel event that ends with an amputation.
It takes both neuropathy and deformity to create an ulcer,3,4 almost universally the sentinel event that ends with an amputation.
In a very large majority of cases those ulcers are of the forefoot and have some relationship to digital deformity, whether direct damage to hammertoes or retrograde deformity leading to increased peak plantar pressures, increased force-time interval and broken-down calluses with subsequent infections. It stands to reason, then, that digital deformities are the thieves that steal the diabetic foot.
Digital deformities are the thieves that steal the diabetic foot.
I assert that it would be most beneficial for us to eliminate these forefoot deformities before they turn into ulcers. Yes, I am suggesting electively surgically correcting forefoot deformities since straight toes lead away from ulcers. This is an excellent way to prevent amputations in the first place. Unfortunately, we don’t have contemporary research studies to back up my assertion, and a study of this type may be tricky and risky to perform. Until this occurs, providers don’t have much support from the literature for this option. As such, too many amputations will occur.
Now, with that said, it is a small jump in logic, and our own experiences show that most of these patients already have deformity and once one toe or ray is amputated the risk of future amputations is significantly elevated.5 One amputation begets another (Figure 1).

With a well-performed transmetatarsal amputation, this is not the case. How can you have a subsequent toe or ray amputation if all of them have already been removed? Instead of performing serial amputations in our sickest patients (Figure 2), with all of the potential complications of peri- and postoperative care, a “one-and-done” procedure can be highly satisfying with improved outcomes.

We will come to the specific technical details to perform a successful transmetatarsal amputation in next week’s issue, but let us finish today’s discussion with some suggestions to help with decision-making (everything leading up to the procedure itself).
- Counseling - This may be the most important aspect for success with this procedure. Without a patient with a full understanding of the procedure, it is likely to fail. My general preoperative consent process includes the following comments: “Our goal is first to save your life by eliminating infection, then to save your leg, and then to save as much function of your foot as possible. With the proper shoes, you will be able to walk after you heal. Losing toes will not affect your overall balance, which is governed by the whole-body. There is an approximately 50% chance you will have some wound healing complication at some point after surgery, but I will be here with you the entire way and we’ll work together to get the best outcome possible.” My approach is realistic but generally positive. I avoid using the phrase “amputation” during the first conversation, replacing it with “removing the toes and knuckle bones.” Euphemisms can spare the patient fear at the start. However, I do use “amputation” on the consent itself.
- Risk - We have to understand that several risk factors will affect overall outcomes and complication rates. It is been well-documented that peripheral arterial disease, renal disease, and uncontrolled diabetes increase the risk of failure.6,7 Whenever possible one should minimize these risks with revascularization, blood sugar control, and overall health optimization. But as we all know, this is often not possible, especially in the face of acute infection in patients with multiple comorbidities, which is why I discuss this topic in detail with patients.
- When to choose the TMA - Patients with severe forefoot infections or global forefoot gangrene are obvious candidates, but more controversial is when to amputate a toe or ray versus the TMA. I’ve made it sound, so far, as if all I do is TMAs, but I still do isolated toe and ray amputations. Isolated 5th ray amputations tend to do well because of its independent range of motion. Similarly, isolated lesser toe amputations do well. First ray amputation research, though, has generally shown that the further proximal the amputation the less positive the outcome.5,6 As a result of these types of repetitive amputations with poor outcomes, the Too Few Toes Principle has been proposed by Armstrong, et al.8 This formula recommends if a hallux plus one lesser toe or two ray amputations need to occur, then a transmetatarsal amputation is indicated. I have found this recommendation to be accurate and reasonable, especially when looking back on past cases of my own and others’ who have tried to salvage as much of the foot as possible, leaving an essentially nonfunctional foot.
The Too Few Toes Principle proposed by Armstrong, et al,8 recommends that if a hallux plus one lesser toe or two ray amputations need to occur, then a transmetatarsal amputation is indicated.
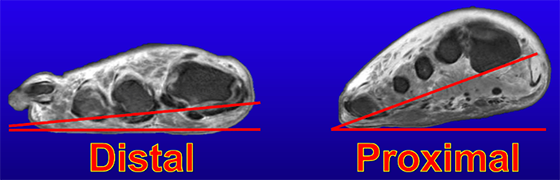
- The goal - When performing a TMA, the surgeon’s goal should be to maintain as much length as possible while removing all nonviable tissue. Mechanically, a very proximal amputation removes the distal aspect of the medial longitudinal arch, creating a biomechanically unsound forefoot varus (Figure 3). Similarly, the residual foot should be entirely plantigrade in all planes. In some cases, especially with proximal amputations, this will necessitate future surgery such as tendon transfers to properly balance the foot. In keeping with this goal of a plantigrade foot in all planes I almost always perform a percutaneous Achilles tendon lengthening with my TMAs. I’m cautious not to overlengthen and have been universally successful with this approach.
Conclusion
With all of these details considered I can say with confidence that this procedure is not something to be feared or avoided but rather embraced by surgeons. A biomechanically sound procedure that reduces the risk of future complications should be viewed with hope – the hope of a patient that continues to walk, remain active in life, and have a fighting chance to battle their health issues into the future.

-
Armstrong DG, Wrobel J, Robbins JM. Guest Editorial: are diabetes‐related wounds and amputations worse than cancer? Int Wound J. 2007 Dec;4(4):286-287.
Follow this link -
Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, Bus SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. 2020 Dec;13(1):1-4.
Follow this link -
Murray HJ, Young MJ, Hollis S, Boulton AJ. The association between callus formation, high pressures and neuropathy in diabetic foot ulceration. Diabet Med. 1996 Nov;13(11):979-982.
Follow this link -
Lavery LA, Peters EJ, Williams JR, Murdoch DP, Hudson A, Lavery DC. Reevaluating the way we classify the diabetic foot: restructuring the diabetic foot risk classification system of the International Working Group on the Diabetic Foot. Diabetes Care. 2008 Jan;31(1):154-156.
Follow this link -
Murdoch DP, Armstrong DG, Dacus JB, Laughlin TJ, Morgan CB, Lavery LA. The natural history of great toe amputations. J Foot Ankle Surg. May-Jun 1997;36(3):204-208.
Follow this link -
Hosch J, Quiroga C, Bosma J, Peters EJ, Armstrong DG, Lavery LA. Outcomes of transmetatarsal amputations in patients with diabetes mellitus. J Foot Ankle Surg. Nov-Dec 1997;36(6):430-434.
Follow this link -
Adams BE, Edlinger JP, Weintraub ML, Pollard JD. Three-year morbidity and mortality rates after nontraumatic transmetatarsal amputation. J Foot Ankle Surg. Sep-Oct 2018;57(5):967-971.
Follow this link -
Miller JD, Zhubrak M, Giovinco NA, Mills JL, Armstrong DG. The Too Few Toes principle: A formula for limb-sparing low-level amputation planning. Wound Medicine. 2014 Feb;4:37-41.
Follow this link -
Schweinberger MH, Roukis TS. Soft-tissue and osseous techniques to balance forefoot and midfoot amputations. Clin Podiatr Med Surg. 2008 Oct 1;25(4):623-639.
Follow this link






























Comments
There are 0 comments for this article