
Practice Perfect 783
An Important Technology You Should Know About
An Important Technology You Should Know About
In the almost 17 years I’ve written the Practice Perfect editorial series, I almost never discuss new technologies. It’s not that I don’t enjoy technology (I’m not a luddite). Rather, I generally remain neutral on the topic and don’t want to influence anyone’s use of one product over another. This time, though, I’m driven to discuss a new technology that offers the opportunity to profoundly affect our podiatric practices and patient care.
I’m driven to discuss a new technology that offers the opportunity to profoundly affect our podiatric practices and patient care.
That product is the SnapshotTM system from Kent Imaging. This is a near infra-red (NIR) imaging system that captures oxygenated and deoxygenated hemoglobin in the skin. Now, before I dive into my experience with this system, I’ll state a couple of disclaimers. I do not receive money or income from Kent Imaging. They have donated two of their systems to my group at Western University for the purposes of research (which I’ll discuss below). I’ve been using their system for about a year in the clinic and the hospital, and I’m very impressed.
I reached out to these folks because, like many podiatrists and other limb preservation specialists, making decisions in the very high-risk patient populations we treat can be challenging. Peripheral arterial disease wreaks havoc on our diabetics and elderly, limiting our ability to help them, and greatly increasing the risk of major limb amputation. This is often a silent disease that goes underappreciated, and it is often difficult to assess the quality of tissue during treatment. Is it safe to do that nail procedure or debride that ulcer? Is there enough oxygen in the skin to heal that amputation? How soon after a revascularization is it safe to do an amputation? These questions and others go largely unanswered, and current technologies such as transcutaneous oxygen measurement are often too difficult, time consuming, and limited to be truly useful. Instead, we need a technology that is point of care, fast, and provides valid information to help us make decisions. Near infra-red imaging promises to be that technology. It’s a game changer.
Making decisions in the very high-risk patient populations we treat can be challenging.

The system itself (Figure 1) is much smaller than earlier devices that used to be as large as Robbie the Robot and is much more portable. About the size of a large shoebox, it has an easy-to-use interface (Figure 2) with a touch screen much like a smart phone. It took their representative about 10 minutes to teach me how to acquire an image, and my residents learn in 5 minutes in the middle of a busy clinic. Acquiring a set of images for one patient takes less than one minute. Office staff could easily be trained to use the system. When starting up the system before taking an image, it requires calibration, much like performing white balancing during an arthroscopic surgery, which only takes a few seconds. Basically, you turn it on, calibrate, and you’re ready to take images. The system is also able to create individual patient reports.


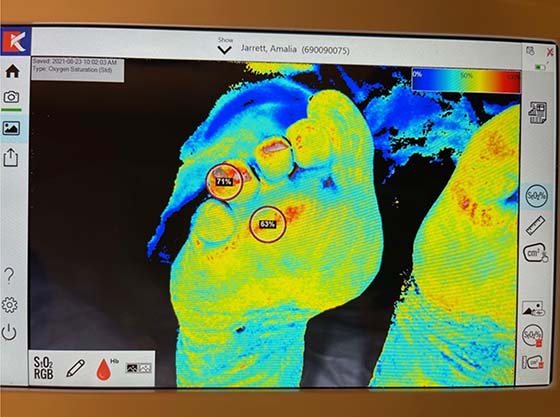
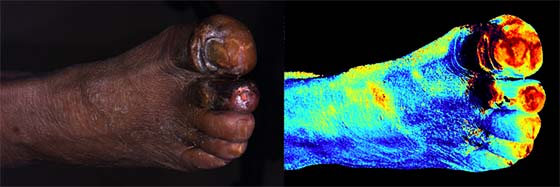
Figures 2a, 2b, 2c. Demonstration case of a 70-year-old patient with a painful periungual callus and initially planned nail procedure. Dorsal and plantar NIR scans demonstrating the data available and the Snapshot interface. Note the blue coloration on the dorsal foot image (2b) indicating low oxygen perfusion of the skin in the patient with peripheral arterial disease.
An intuitive color spectrum provides quick feedback that is easy to explain to patients with the red spectrum indicating increased oxygen and blue spectrum showing deoxygenation. The system also provides an oxygen percent determination on all areas of the image with a touch of the screen.
Red spectrum indicating increased oxygen and blue spectrum showing deoxygenation.
Figure 2 shows an illustrative case. This was a patient of mine on which I was planning a nail procedure for a painful periungual callus. Preoperatively, I scanned the foot and found the images shown. The blue color on the dorsal foot demonstrates poor tissue perfusion (anterior tibial angiosome occlusion) with improved plantar perfusion. Note the circled percentages on the plantar view showing a hyperemic response at the 4th digit. TCOMs do not allow us to determine perfusion at multiple specific anatomic locations simultaneously, but this new technology does. This patient underwent successful angioplasty with orbital atherectomy of the anterior tibial artery, and I was able to perform my procedure without complications.
TCOMs do not allow us to determine perfusion at multiple specific anatomic locations simultaneously, but this new technology does.
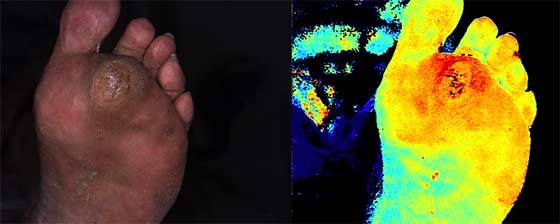
Figure 3 demonstrates another case in a patient with a sub-2nd metatarsal head diabetic neuropathic ulcer with adequate tissue perfusion. Note the deep orange coloration of the plantar forefoot and red color in the periwound and within the wound bed indicating neovascularization of the wound bed. Incidentally, it’s interesting to note how much inflammation there is in this wound environment that would have otherwise gone unnoticed clinically.
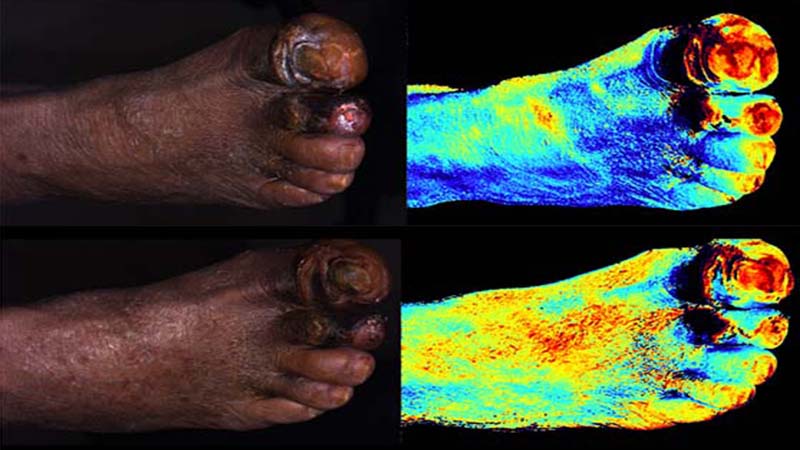
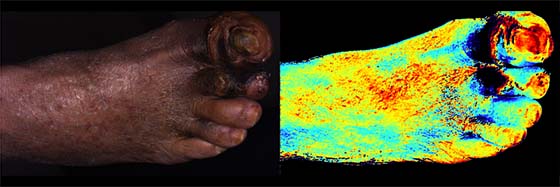
The potential power of this technology is shown in Figure 4. This patient with diabetes, severe PAD, and gangrene of two digits was at high risk for a major limb amputation. His initial scans (Figure 4, top) show low arterial perfusion. He was referred to a vascular surgery colleague and successfully underwent endo-revascularization and hyperbaric oxygen therapy, successfully healing a transmetatarsal amputation. The Snapshot system allowed me to have a better understanding of the quality of tissue we had to work with and empowered me to guide his pre- and postoperative care to a successful outcome.
Now, nothing is perfect, so to remain balanced here, I’ll make a few critical comments. This technology does not yet exist as an application that can be used on a smart phone. Carrying the case may feel a bit cumbersome, especially in the hospital, but it sure beats rolling devices on wheels. The system is not cheap, but I’m told there is a new billing code that allows reimbursement. Unlike TCOM measurements, NIR imaging requires further validation, which is why my group is currently helping with research. Our current research is aimed at using this technology to make clinical decisions, so we are examining baseline oxygenation percentages in the healthy population, using these percentages to stratify outcome risks, and determining amputation levels. We anticipate that our research will demonstrate the power of near infra-red imaging to help our patients and improve outcomes in a very high-risk population. I’m excited to see where this technology will lead in our fight against PAD.




























Comments
There are 0 comments for this article