
Practice Perfect 803
Pain Scales: Are They Legit?
Pain Scales: Are They Legit?
“Dr X, my foot really hurts.”
“I’m sorry to hear that,” says Dr. X. “On a scale of 0 to 10, with 10 being the worst possible pain, how would you rate your pain?”
“It’s an 11. Yes, definitely an 11.”
I’m not sure how many times in my practice I’ve experienced something like the above conversation. Pain is the most common reason patients see physicians, yet it is a subjective complaint with many complexities. We call pain the 5th vital sign, and we are instructed to assess the severity of pain, but I often find this method to be challenging due to its subjectivity.
Pain is the most common reason patients see physicians, yet it is a subjective complaint with many complexities. We call pain the 5th vital sign.
It’s also not uncommon to speak with a patient who says they have 10/10 pain, sitting quietly in the chair, apparently comfortable, and smiling. When I explain a 10/10 would be excruciating pain that has one ask to have their leg amputated, the patient will often answer, “Oh, yes, that’s right. Ten out of ten.” That’s not 10/10 pain.
I’ve seen 10/10 pain. I once had a young patient with complex regional pain syndrome after an ankle sprain with horrific pain, shaking, sweating, grimacing, and intermittently crying. This poor girl would have allowed us to remove her leg right there if it would have stopped her pain. That experience was the benchmark against which I evaluate most patients, subjective as this may be.
Obviously, some patients may describe these numbers inaccurately for a variety of reasons, some legitimate and others not. Patients often experience pain in different ways with some rolling around and others stiff as a board. Certain types of pain – think paresthesias versus achy muscle pain as an example - are experienced differently and may be tolerated to different extents. Some patients simply have high pain tolerances, and others (a thankfully a small number) are seeking secondary gain.
This incredibly complex interplay of physiology, psychology, and human interaction makes me wonder just how it is possible to boil all this down to a simple number. How accurate is the numeric rating scale, and are there reasonable alternatives?
How accurate is the numeric rating scale, and are there reasonable alternatives?
History of the VAS Scale
Before we get to that, I can’t help but review a bit of the history surrounding these scales. The Visual Analogue Scale (VAS) in common use today was originally created in the emergency department for people who were not able to speak the dominant language of their location.1 It’s termed “visual”, but it is actually a 100 mm line where patients mark their pain level with the left side no pain and the right maximal pain. It is termed “analogue” because the line is continuous rather than discrete. Using a 0 to 10 scale is not the visual analogue scale but is rather a numerical rating score. As we’ve all seen, combining the linear, ideographic (pictures) and numerical scales like the image below is often used in clinical practice.
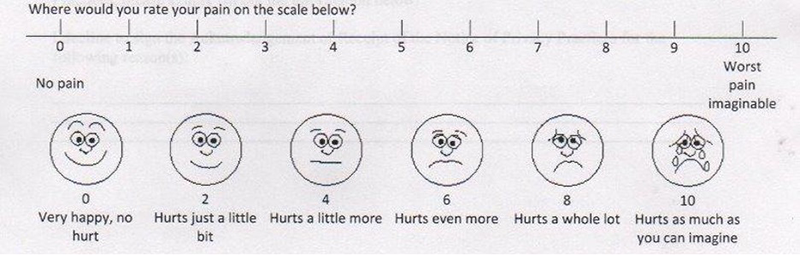
Keep in mind that all of these methods are descriptors of pain intensity alone and do not characterize other aspects of pain such as type, location, situations, and modulating factors, among others. By no means does any scale replace a detailed history and physical examination.
Is the VAS Accurate?
A systematic review that included 54 papers found numerical rating scales and visual analogue scales to have good compliance and agreement with control methods and thus had reasonable applicability in a variety of pain settings.2 The authors also stated that more research needs to be done to determine if certain anchors (the descriptors at either end of the scale – “no pain” versus “worst pain imaginable”, for example) or the methods by which patients can respond still require further research. Not surprisingly, the authors noted that the VAS scale (with its several iterations) was the most studied pain rating scale.
Important for those of us in clinical practice, visual scales like the VAS have been found in several older studies from the 1970s era to be as accurate as numerical rating scales. It appears the literature supports the use of either method when determining pain intensity, though some prior research indicated an issue with the complexity of some of the scales. As some patients may find it difficult to use some scales, even with clear instructions, it is suggested to keep the pain assessment method as simple as possible.
Here’s an option for those of you interested in a relatively easy method that differs from the typical numerical rating scale. Print something like the image below on a piece of paper. Make sure the line is 100 mm in length. Don’t put hash marks on the line. Add the faces or leave them off as you see fit. Have the patient indicate the location on the line that best describes their pain level. Measure the length of the line at the spot the patient indicated in millimeters. That number is the VAS. If you like to use a 10 scale, just divide the result by 10. For example, if the patient’s mark was at 85 mm then they have 8.5 out of 10. This can easily be added to a patient intake form, or it can be placed on a card medical assistants use when rooming patients to make this a faster process.
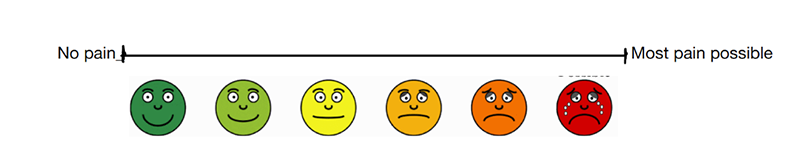
It is also possible to digitize a scale like this with a moveable cursor controlled by the patient that indicates the pain intensity.
Are There Alternatives?
A large number of alternative assessment methods have been developed over the years. For example, the American Orthopedic Foot and Ankle Score (AOFAS) and the American College of Foot and Ankle Surgeons (ACFAS)3,4 systems have both been validated. These two systems are different from the VAS in that they both include a physician component and are thus considered “physician reported” rather than patient reported, and they include an objective component (though the objectivity varies somewhat). Other systems, such as the Foot Function Index, also exist which attempt to assess various aspects surrounding pain and function more comprehensively. I applaud the creators of both the AOFAS and ACFAS scoring methods for their more objective multidimensional assessments, but these systems may be too cumbersome for use in daily practice and appear to have been in great use in the research realm. I’m not certain if my last comment is actually true as I have not attempted to use one in practice.
For those wishing a more systematic and comprehensive assessment of functional outcomes, I suggest taking a deeper look at the ACFAS scoring system. I plan a trial use of the ACFAS system in my Western University practice and will report on how it went. Watch for that in the future! Regardless, it’s satisfying to know that our current common methods to quickly determine pain intensity (if not function) are reasonably valid. Each of us should explore our own methods of assessing pain, see what works best with our practices, incorporating those into patient care to evaluate our outcomes and better understand our patients’ pain.
Best wishes.

Jarrod Shapiro, DPM
PRESENT Practice Perfect Editor
[email protected]

-
Hayes MHS and Patterson DG. (1921) Experimental development of the graphic rating method. Psychological Bulletin. Vol 18, 1921, 98-99.
Follow this link -
Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, Fainsinger R, Aass N, Kaasa S, European Palliative Care Research Collaborative (EPCRC). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011 Jun;41(6):1073-1093.
Follow this link -
Cook JJ, Cook EA, Rosenblum BI, Landsman AS, Roukis TS. Validation of the American College of Foot and Ankle Surgeons scoring scales. J Foot Ankle Surg. 2011 Jul 1;50(4):420-429.
Follow this link -
Thomas JL, Christensen JC, Mendicino RW, Schuberth JM, Weil LS, Zlotoff HJ, Roukis TS, Vanore JV. ACFAS Scoring Scale user guide. J Foot Ankle Surg. Sep-Oct 2005;44(5):316-335.
Follow this link






























Comments
There are 0 comments for this article