
Practice Perfect 644
Is Podiatry a Surgical Specialty? – A Response
Is Podiatry a Surgical Specialty? – A Response

Dr Alan Sherman recently posed an important question to the profession in PMNews and Barry Block, DPM accompanied it with a survey asking the question, “Is podiatry a surgical subspecialty, or is surgery a sub-specialty of podiatry?” This question comes on the heels of the very important Council on Podiatric Medicine’s call for comments during their rewrite of the 320 document that defines the rules for podiatric residency programs. Dr Sherman’s question brought a number of interesting responses, and it probes an issue topical to contemporary podiatry: our multifaceted identity.
The poll results are as follows:
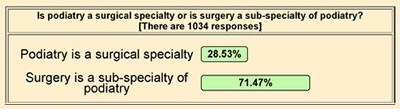
These results demonstrate the respondents’ overwhelming view that podiatry is NOT a surgical subspecialty but rather a profession with a surgical component. My general opinion is to agree with the majority, but there are nuances to this topic that should be explored.
Why Does This Question Matter?
To some this question may seem academic, but it truly gets to the heart of many of our problems as a profession. Since podiatry acquired a surgical aspect years ago, we have been on a trend toward an ever-increasing surgical role while relinquishing many of our nonsurgical aspects (the schizophrenic identify referred to by some). Let me say at the outset that I’m a surgically trained pod, and surgery is an important part of my professional life. I don’t think we should give up surgery and, in fact, advocate that we ought to continue expanding the procedures in our scope (for example, we should be allowed to do below knee and Symes amputations, which is not permitted in many states).
Do we all need to be advanced surgical specialists? I don’t think so.
On the other hand, we should not lose the original components of podiatry (biomechanical-related treatments, wound care, office-based practice, etc). Both aspects are simply two sides of the same coin, and we should use both surgical and nonsurgical methods to obtain the best patient outcomes possible. Does it mean we all individually have to do both? I don’t think so. The same or better outcomes can occur with podiatrists who have focused expertise.
Advanced Surgery as a Sub-Specialty of Podiatry
If advanced foot and ankle surgery is a sub-specialty of podiatry, then our podiatry schools and residency training should reflect this identity. I think it’s pretty clear that this is not currently the case. For example, of the 1,000 clinical encounters required of our residents during training, only 75 of them are biomechanical examinations. This compares with a minimum 400 surgical procedure requirement. Similarly, our community appears to value surgeons over clinicians.
If advanced foot and ankle surgery is a sub-specialty of podiatry, then our podiatry schools and residency training should reflect this identity. I think it's pretty clear that this is not currently the case.
Don’t agree? Go to an ACFAS conference and see the number of attendees and vendors. There’s a reason this is one of our largest yearly conferences. This is all despite the fact that upwards of 70-80% of most of our practices are nonsurgical.
The Dual Track Third Year for Podiatric Residency Education
To rectify these problems, Dr Sherman has advocated for a revised model of residency training in which residents with the most potential to be advanced foot and ankle surgeons are tracked into an advanced surgical third year (with the possible creation of other 3rd year emphases such as wound care, biomechanics, etc). He makes a convincing argument, and on the face of it, I agree. I don’t take issue with changing podiatric education to focus on our strengths (surgically oriented folks becoming surgeons and others becoming clinicians). I do have a concern with the details and possible ramifications of this change.
Consequences to Consider
I see four major consequences or hurdles to consider:
- Creation of a confusing identity to the medical profession.
- Residency conversion difficulties and unanticipated consequences.
- The surgery versus clinical hierarchy.
- Incorporating the general practice podiatrist into the current job market.
Confusing Identity and Characteristics for the Profession
In the not so distant past, there was an alphabet soup of podiatric residencies: primary podiatric medical residency (PPMR), podiatric surgical residency (PSR) 12, 24, 24+, 36, rotating podiatric residency (RPR), and primary orthopedic residency (POR). With all this variety, it seemed few within the podiatric profession understood the different training programs, much less the rest of the medical profession. One of the benefits of the profession’s move toward a more standardized residency training is the ability to clearly advertise our training to the medical community. It remains a challenge to explain what we do to other providers, and I fear going back to a more variably-appearing training could be damaging.
Residency Conversion Difficulty and Reactions
I’m not certain that our residency programs are structured to easily convert to a format that redirects the residents to an advanced surgery 3rd year as their programs progress. Each residency has a certain amount of resources available, with some programs being more surgical, while others have a mixture of surgery and clinic. The objectives, outcomes, and assessment methods would need to differ to some extent (which, again, would increase variability to the outside world). These differences in tracks could make it very difficult for program directors to convert their programs.
Perhaps somewhat obvious, one might ask if a three-year residency is actually necessary for those not on the surgery track. If the third year is dedicated to specialty aspects such as surgery or wound care, and those who do these subspecialties need only two years of general practice podiatry training before practice, can we conclude that two years is actually enough training for general podiatric practice?
My answer to this question is absolutely not. Residency training needs to remain three years because as a resident transitions from first year to the third year, how they interpret their experiences changes and matures. This is especially true for those programs that chose surgical procedure assignments by year (third years doing the larger reconstructive procedures with first years doing smaller surgeries). If a majority of surgical training occurred in the 3rd year, would this be enough for a resident’s understanding to mature?
Hierarchy Hassles – What Do Students Want?
We also need to address the unfortunate hierarchy of surgery over clinical practice head on. Despite the results of the poll above that examined practicing provider opinions, many of our students still want to be surgeons, despite the unreality of this desire. I would be interested in seeing the results of a poll of the students in our nine podiatric colleges. If a majority of students actually want to be surgeons, then a change in residency structure could affect how applicants chose residency programs. Given how competitive residency programs are – even in the face of less programs versus more applicants – I’d be concerned to see what behavioral changes would happen. I can also envision a hierarchy created within residency programs with the surgical residents on top of the others.
Where is the Nonsurgical Job Market?
The next concern is about available job positions after residency graduation. It appears currently that having a heavily surgical training improves a graduate’s chances at obtaining a higher paying job – at least initially. An example of this is a job with an orthopedic practice that typically pays more and the Kaiser Foundation that pays its surgical podiatrists higher than the nonsurgical ones. In private practice, this dichotomy likely holds a little less true. However, a graduate with both heavily surgical training plus the ability to run a clinic is the most competitive young podiatrist.
What jobs would be available to our nonsurgical colleagues? What extra skills would they bring to make them marketable? As it stands now, I would not want to be a nonsurgical pod looking for a job. Let me make it clear that I’m not saying a clinical podiatrist is inferior in any way to a surgical podiatrist. But what does seem clear in the current job market is that a surgically trained podiatrist who is able to do at least some aspect of clinical medicine is a more desirable applicant for a job.
A Solution - The General Practice/Advanced Surgeon Partnership Model
There is a potential solution to this, which I’ve written about previously: pair nonsurgical and surgical podiatrists in clinical practice. The clinical podiatrist spends the majority of their time in clinic, and, when a patient needs surgery, sends that patient to their surgical partner. Each focuses on his or her expertise with increased patient volume within that expertise. Both would be contributing equally to practice, so should be equally compensated.
The bottom line here is if we make the potentially beneficial recommended changes to our residencies that Dr Sherman suggests, this might create an unwelcome confusion about the profession, would require changes in how residencies function that may be too burdensome, may cause a worsening of the current nonsurgical versus surgical podiatrist dichotomy, and possibly leave our nonsurgical brethren with uncertain futures. These potential ramifications should be considered before we undertake major changes to how our postgraduate education is structured. Perhaps our first step should be to address our podiatric identity crisis. But that’s another debate.





























Comments
There are 0 comments for this article