
Practice Perfect 751
Let’s Talk TMA - Technique Tips - Part 2
Let’s Talk TMA - Technique Tips - Part 2

Last week in Practice Perfect 750, we discussed the important role of the transmetatarsal amputation (TMA) when taking care of those unfortunate patients with forefoot complications of diabetes. Rather than consider this amputation a last resort, surgeons should embrace the functional nature of the residual foot after the TMA…when the procedure is done correctly. Here are some tips I have found to markedly improve the long-term durability and success of the TMA.
- Consider an adjunctive Achilles Lengthening (TAL) - Let’s start right off with some controversy. I do a percutaneous Hoke triple hemisection Achilles lengthening with every TMA. It’s entirely anecdotal, but in 16 years of practice I have never caused a plantar heel ulcer from overlengthening. I do the procedure before the TMA unless the foot is significantly infected, such as in cases of necrotizing fasciitis. I have not experienced postop infections of the TAL site despite the level of foot infection. Nor have I caused a rupture or overlengthening by doing the TAL before the amputation. The patient is placed in the supine position and an assistant raises the leg and maintains moderate dorsiflexion of the foot. The stab incisions are placed at 2, 5, and 8 cm proximal to the Achilles insertion according to Roukis . This takes about 60 seconds and is easily done with a 15 blade (not an 11 blade due to its longer blade length) without a tourniquet. It can be sutured or steri-stripped at surgeon’s preference. The tendency is to under-lengthen initially and then to push hard when dorsiflexing the foot. This is a mistake. The surgeon should only have to apply a gentle dorsiflexion force to properly lengthen the tendon fibers. These patients are kept entirely nonweightbearing for 4 weeks after surgery (assuming it’s safe to walk the amputation site at that time).
- Incision and dissection tips - Many textbooks draw the incision with the dorsal aspect meeting the plantar flap at 90 degrees. This is a good way to create dogears. Instead, taper the corners as shown in Figure 1. For those new in practice, leave as much length to the flaps as possible and remodel the extra length when ready to close. Remember, once that tissue is removed, you can’t put it back! I like to plan my dorsal incision to line up almost exactly with the dorsal location of the metatarsal osteotomies; this leads to a firm, not too tight or loose amputation stump that is well-padded and not floppy. Remember to never bevel the skin incisions – stay perpendicular to the skin to prevent devitalizing the incision. During the dissection, make efficient long strokes (rather than short sketches) to maintain one uniformly thick plantar flap that doesn’t have cuts in multiple layers. Small sketching motions lead to freely hanging pieces of tissue at risk for devitalization.
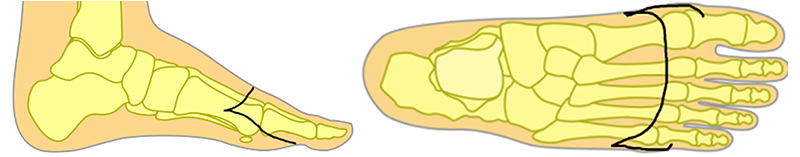
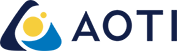
Figure 1. Incisional appearance to decrease the risk of post-incision dogears. - Maintain as much residual foot length as possible - The best TMA has bone resection just proximal to the metatarsal heads. However, this is not always possible given the amount of bone and/or soft tissue involvement. If the amputation ends up proximal (near the metatarsal bases), then be ready for additional procedures to balance the foot, either during the index amputation (generally not what I like to do) or in a staged fashion later. I’m partial to a posterior tibial full tenotomy to remove residual adductus, a full tibialis anterior transfer (not split) to the lateral cuneiform or the cuboid (depending on how much eversion is desired), and sometimes a peroneal transfer to augment eversion (Figure 2). Here’s an extra tip: if it’s possible to preserve metatarsal length, but there is not enough soft tissue to full cover the amputation (such as if dorsal soft tissue has been lost), then don’t shorten the amputation. Instead leave it long with a wound that can be closed later using negative pressure and skin grafting or other wound healing methods.

Figure 2. A well-balanced TMA after tibialis anterior transfer,
posterior tibial tenotomy, and TAL. - Bevel the bone cuts distal to proximal - Aim for approximately parallel to the weightbearing surface (Figure 3). This will change based on the foot type. A cavus foot type can have the cuts angled almost straight flat while doing the same with a planus foot will lead to the cut running too far down the shaft and not exiting. One should never make the cut perpendicular to the metatarsal – this will lead to focal increases in plantar pressure and doom the patient to future ulcers.

Figure 3. Beveled metatarsal cuts to reduce plantar pressures. - Focus on the parabola - It is highly important to create an anatomic parabola with all of the metatarsals gradually shortening from a slightly longer second metatarsal (Figure 4). I like to start with the second metatarsal and line the cuts up to its medial and lateral corners, but this is personal preference, and different surgeons like different approaches. It doesn’t matter as long as a parabola is created in an efficient manner. In some cases, one metatarsal may already be very short due to prior ray amputation. Instead of creating a very proximal TMA, I like to create a parabola using the remaining four metatarsals, adjusting the length accordingly. This is not as good as a five-metatarsal parabola but remains sufficient for a durable amputation.

Figure 4. Parabolic shape of the metatarsal osteotomies reduces
postoperative focal plantar pressures. - Watch out for arterial danger zones - There are two primary areas in the plantar flap of which to be careful during your dissection: the central area and just plantar to the first metatarsal stump. If cut, both areas will bleed heavily, so I try to avoid them when possible to decrease blood loss.
The final tip has to do with post-healing shoe gear. Patients can ambulate very well with a stiff soled extra-depth shoe with trilaminar insole and forefoot filler. Additionally, a rigid shank placed under the insole will prevent the shoe from bending in half as the patient propels (most suppliers provide these on request), and a rocker sole simulates propulsion in those patients determined to be at low risk for falls. Checking proprioception is always a good idea. Flat-bottomed outsoles are better for patients with poor balance.
The devil is very much in the details when performing the transmetatarsal amputation, but if properly executed, this procedure may yield excellent durable outcomes with a functional foot and fully ambulatory patient.

-
Schweinberger MH, Roukis TS. Surgical correction of soft-tissue ankle equinus contracture. Clin Podiatr Med Surg. 2008 Oct;25(4):571-585.
Follow this link



























Comments
There are 0 comments for this article